When it comes to maintaining a healthy, functional body, it’s easy to overlook the pivotal role of certain muscles in everyday movement and long-term stability. One such muscle is the gluteus medius. At Melbourne Massage and Treatment, located in Fitzroy North, I see many patients who either love running or love to hit the gym but are not aware of the importance of this muscle for their activity.
What is the Gluteus Medius?
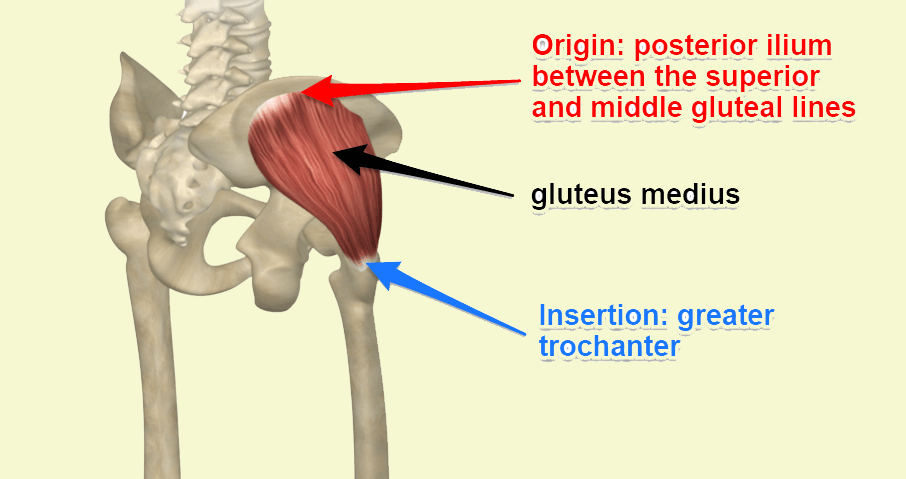
The gluteus medius (GM) is one of the three primary muscles of the gluteal group, located in the upper part of the buttock. 
Here is a breakdown of its anatomy:
Origin: the gluteal surface of the ilium
Insertion: lateral surface of the greater trochanter
Innervation: dorsal branches of the L4, L5, and S1
Actions: Abduction and medial rotation of the lower limb.
It stabilises the pelvis.
Thanks to its positioning, the GM plays a vital role in controlling pelvic movement, specifically in the stabilization of the pelvis during various motions like walking, running, or standing on one leg.
More Information About Gluteus Medius actions
The GM serves several essential functions that directly affect the stability of the hip and lower body:
- Pelvic Stabilization: One of its primary roles is preventing the pelvis from tilting excessively to one side when you move, especially when you’re walking or running. If the gluteus medius isn’t working properly, the opposite side of your pelvis may dip downward, leading to an imbalance and compensatory movements that strain other parts of the body.
- Hip Abduction: The gluteus medius helps to move the leg out to the side, away from the body. This movement, known as hip abduction, is crucial for activities that require lateral movement, such as stepping sideways or maintaining balance while performing physical tasks.
- Internal and External Rotation: The gluteus medius also assists with the rotation of the hip joint. Depending on which fibers are activated, it helps with both internal and external rotation of the thigh. This is essential for maintaining control and precision in movements.
- Postural Support: The gluteus medius muscle helps keep the pelvis level when you’re standing on one leg. Without proper activation of this muscle, one hip might drop, affecting posture and causing misalignments in the spine and lower back.
The Role of the Gluteus Medius in Hip Stability
Why is the GM so important for hip stability? Simply put, this muscle acts as the stabilizer of the pelvis. Without a properly functioning gluteus medius, other muscles and joints are forced to compensate for the lack of stability, leading to overuse and strain. For example, improper GM function can result in excessive stress on the knees, lower back, and even the ankles, which can lead to pain, discomfort, and injury.
Clinical implications are vast, especially for athletes and individuals who regularly engage in physical activities. Hip instability can result in difficulty performing simple tasks like walking or climbing stairs, and over time, it may contribute to chronic conditions such as hip osteoarthritis.
A common painful presentation that we see in athletes but also the everyday patients is Greater Throcanta Pain Syndrome (GTPS), which is characterised by the side hip pain. This presentation results from a GM tendon irritation.
Signs of Weak or Dysfunctional Gluteus Medius
Here are some common signs that your gluteus medius may need attention:
Pain in the hip or lower back: Since this muscle is integral to proper alignment, dysfunction often manifests as discomfort in the hips or lower back.
- Difficulty balancing on one leg: Struggling with stability when standing on one leg may indicate weak gluteus medius muscles.
- Shifting or limping while walking: A noticeable shift or limp while walking can point to weakness in the gluteus medius, causing the body to compensate and disrupt your gait.
How can Gluteus Medius impact your run?
The gluteus medius is crucial for runners as it stabilizes the pelvis, controls hip movement, and ensures proper alignment during running. This muscle prevents excessive pelvic tilting, reduces side-to-side sway, and helps maintain efficient running form, thereby lowering the risk of injuries such as knee pain, IT band syndrome, and lower back discomfort. A weak or dysfunctional gluteus medius can lead to compensatory movements, affecting performance and causing imbalances.
How Melbourne Massage and Treatment Can Help
At Melbourne Massage and Treatment, as a clinical myotherapist, I focus on treatment designed to address muscle pain and dysfunction through a variety of techniques. One of the key areas of focus is to create a treatment plan that works for your presentation based on your clinical history.
Here is a breakdown:
1. Assessment and Diagnosis: I would conducts a thorough assessment to identify if the gluteus medius is underperforming, weak, or compensating due to other musculoskeletal issues. This involves a combination of posture analysis, movement patterns, and targeted strength tests.
2. Myotherapy Treatment Techniques: I will use various techniques, including trigger point therapy, Dry Needling, myofascial release, and deep tissue massage, to release tension in the gluteus medius and surrounding muscles. This helps to restore proper function, reduce pain, and improve mobility.
3. Rehabilitation and Strengthening: After addressing any issues, we will work to develop rehabilitation strategies, including targeted strengthening exercises for the gluteus medius and other muscles that surround the pelvic, lower back and leg area. These exercises aim to restore proper muscle activation and prevent future imbalances.
4. Injury Prevention: In order to prevent further injury, we will set a target of strength that you want to achieve with your sports activity, and we will do our best to hit that target. Be mindful that based on your presentation, the target could extend from a few weeks to several months.
The Takeaway
The gluteus medius muscle is far more important for hip stability than many people realize. Its role in maintaining pelvic alignment and controlling movement is essential for pain-free mobility, proper posture, and long-term musculoskeletal health. Whether you’re dealing with hip pain, experiencing difficulty with balance, or want to prevent future issues, understanding and caring for your gluteus medius muscle is crucial.
At Melbourne Massage and Treatment in Fitzroy North, I commit to providing personalized, effective treatment options to help restore balance, alleviate pain, and enhance your overall physical well-being. If you suspect your gluteus medius may contribute to discomfort or instability, don’t hesitate to book an appointment and start your journey toward better hip stability today.
FAQ: Gluteus Medius and Hip Stability
Q: What is the GM, and why is it important?
A: The GM is a muscle located in the upper part of your buttocks. It plays a crucial role in stabilizing your pelvis, especially when walking, running, or standing on one leg. This muscle helps with hip abduction, internal and external rotation, and maintaining posture. Proper function of the GM ensures better hip stability and reduces the risk of injury.
Q: How does the GM affect movement?
A: The GM stabilizes the pelvis during movement, preventing excessive tilting and maintaining a balanced posture. It is essential for activities that require side-to-side movement or balancing on one leg, such as walking, running, or climbing stairs.
Q: Can weak GM muscles cause pain?
A: Yes, weakness or dysfunction in the GM can lead to various problems such as hip or lower back pain. When this muscle is not functioning properly, other muscles or joints must compensate, which can lead to pain, imbalances, and even injury over time.
Q: What are the signs that my GM might be weak or dysfunctional?
A: Common signs of a weak GM include:
- Hip or lower back pain
- Difficulty balancing on one leg
- A noticeable limp or shifting while walking
- Difficulty maintaining posture during activities like running
Q: How does the GM impact running?
A: The GM is crucial for maintaining proper pelvic alignment and stability while running. A weak GM can lead to excessive pelvic tilting, inefficient movement patterns, and increased risk of injuries such as knee pain, IT band syndrome, and lower back discomfort.
Q: How can Melbourne Massage and Treatment help with GM issues?
A: At Melbourne Massage and Treatment, I provide personalized treatment plans to address any GM dysfunction. This includes:
- Thorough assessment and diagnosis
- Myotherapy techniques (trigger point therapy, dry needling, myofascial release, deep tissue massage)
- Rehabilitation and strengthening exercises to restore muscle function and prevent imbalances
- Injury prevention strategies to help you maintain strength and stability for your specific activities
Q: How long will it take to see improvements in my GM strength?
A: The timeline for improvement depends on the severity of the issue and your individual presentation. Some individuals may see improvements within a few weeks, while others may need several months of rehabilitation and strengthening exercises to reach optimal function.
Q: Is the GM important for posture?
A: Yes, the GM is vital for maintaining proper posture. When this muscle is weak or dysfunctional, it can cause one hip to drop, leading to misalignments in the spine and lower back. Strengthening the GM can help prevent postural issues and contribute to better overall body alignment.
Q: Can the GM contribute to knee or ankle pain?
A: Yes, improper function of the GM can cause compensation in other joints, including the knees and ankles. This can lead to overuse, strain, and discomfort in these areas. Strengthening the GM helps to reduce the load on the knees and ankles, preventing pain and injury.
Q: How can I strengthen my GM?
A: Strengthening the GM involves targeted exercises, such as side-lying leg lifts, clamshells, squats, lunges, and hip abductions. Working with a myotherapist can help you develop an appropriate rehabilitation plan that’s tailored to your needs and goals.

Giovanni La Rocca
Giovanni moved to Melbourne, Australia, from Italy in 2008 and became a citizen in 2017. He started studying massage therapy in 2016, then completed a Bachelor of Health Science in Clinical Myotherapy in August 2024. During those years, he also specialised in Thai Massage and Manual Lymphatic Drainage for presentations like Lipoedema and Lymphoedema. Nowadays, he runs his clinic in Fitzroy North, Melbourne, where he integrates movement therapy into his practice to enhance overall well-being. He also values meditation, having completed several Vipassana courses. Committed to continuous learning, he aims to share his expertise in integrated therapies to help others achieve balance and resilience.