Musculoskeletal pain can be complex, and orthopedic tests and hands-on treatment, sometimes, can be a limited tool to individualise what is happening with the body’s internal structure. Indeed, there are times when a deeper look is required to ensure we are on the right path. This is where body scans imaging comes into play to identify presentations like tendinopathy, bursitis, ligament tear or other underlying conditions. The Role of Body’s Scan in Diagnosing Pathology Body scans include a series of imaging technologies, such as ultrasound, x-ray, MRI, to name a few. Ultrasound is a highly effective imaging tool used to assess soft tissue structures in real-time. Unlike X-rays, which primarily show bone, ultrasound provides detailed images of muscles, tendons, bursae, and ligaments. This makes it an excellent tool for diagnosing conditions such as: Tendinopathy – A chronic condition involving tendon degeneration due to overuse or injury. Bursitis – Inflammation of the bursae, the small fluid-filled sacs that reduce friction between tissues. Those tissue types are found along different body joints, like the shoulder and the hip. Ligament Tears – Partial or complete tears of ligaments, often occurring after trauma or excessive stress. Baker’s cyst – is a fluid-filled swelling that forms behind the knee, often resulting from knee joint conditions like arthritis or meniscal tears, causing discomfort and limited mobility. When we are suspicious of one of those presentations, due to positive results obtained by orthopedic test and medical history, including mechanism of injury, we attempt a recovery process, based on the type of injury, symptoms, and other relevant information. Along this recovery process, we may start with isometric exercises. If, with the first 6 weeks, and a series of sessions, 3 to 4 sessions with this time frame, we still don’t see a major recovery, then we may want to get extra investigation ongoing via an ultrasound scan, which can clarify the underlying pathology. It allows us to confirm or rule out certain conditions, ensuring that treatment strategies are aligned with the actual tissue damage (if any is present). On the other hand, based always on the individual case, we could also require X-rays, which are often more helpful in diagnosing conditions related to the bones, such as arthritis or fractures, as they provide a clear view of bone structure and joint spaces. MRI is a scan that is used for Brain imaging, and when the investigation needs higher details, like when looking at the spine or a joint that via ultrasound was not giving any sign of issue. Ultrasound is also comparable to MRI, as it is faster, easier to deliver, and has fewer complications. How can myotherapy treatment help recovery from what a body scans would show? As we already discussed in another blog, Myotherapy is a practice that looks into the well-being of the skeletal muscle structure. To understand what can be done about a painful presentation, we would initially take a detailed clinical history, then look into objective measurements, such as your movement and body presentation. Given the result we can obtain, we would build up a treatment plan which includes: Hands-on Treatment – Techniques such as deep tissue massage, myofascial release, and dry needling can help reduce pain and improve mobility. Exercise Prescription – Strengthening and mobility exercises help restore function and prevent future injuries. Load Management Strategies – Proper guidance on activity levels ensures tissues heal without excessive strain. That management technique would then be combined and adjusted around the scan’s results. Here are a few examples: Bursitis: If a bursitis is confirmed, medications may be given to reduce the inflammation of the bursa, for that, we concentrate on MLD treatment to further reduce the inflammation and exercises to build strength on the structure that needs support. Ligament tear: When talking of ligament tear, the healing time can dilagate to months if not also a year, so we know now why the 6 weeks program may was not as responsive. We will keep focusing on the strength of the muscle that surrounds the specific joint, and use hands-on treatment to boost blood to the area affected. Arthritis: Medication or dietary change may be put in consideration for pain management and inflammatory reduction. Also in this case, MLD can be used to manage the pain response, and exercises for mantain movement in the affected joint/s. When Should You Consider an Ultrasound or other body scans? If you experience ongoing pain, swelling, or restricted movement that is not improving with therapy, an ultrasound or other scan helps identify the cause. This can prevent prolonged discomfort and allow for a more targeted treatment approach. At Melbourne Massage and Treatment, in Fitzroy North, we aim to provide the most effective care possible. If you’re dealing with persistent musculoskeletal pain, book a consultation with Giovanni today. Together, we’ll determine the best action to get you back to optimal function. Frequently Asked Questions (FAQs) About Musculoskeletal Pain and Body Scans Imaging 1. What are body scans, and how do they help diagnose musculoskeletal pain?Body scans include imaging technologies such as ultrasound, X-ray, and MRI. These scans help diagnose soft tissue injuries (like tendinopathy, bursitis, and ligament tears) or bone-related conditions (such as fractures or arthritis). They provide a clearer picture of what might be causing pain, inflammation, or restricted movement. 2. Why is ultrasound commonly used in diagnosing soft tissue injuries?Ultrasound is highly effective for real-time imaging of soft tissues like muscles, tendons, bursae, and ligaments. It helps diagnose conditions such as tendinopathy, bursitis, and ligament tears, providing a dynamic view of the area being studied without the need for invasive procedures. 3. When should I consider getting an ultrasound or other scans for my injury?If you’re experiencing persistent pain, swelling, or limited mobility that isn’t improving with initial therapy (such as exercises or hands-on treatment), it might be time to consider an ultrasound or other scans. These can help identify the underlying cause of your symptoms and allow for a more targeted treatment approach. 4. How do orthopedic […]
Tag Archives: tear
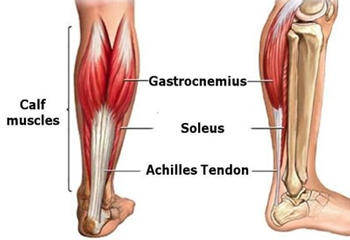
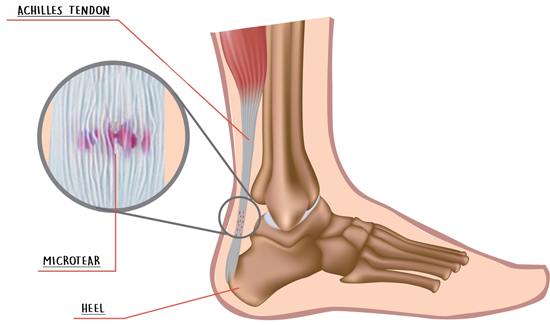
Achilles tendinopathy is a condition that manifests on the lower portion of the calf and is caused by overusing the muscle of this region, such as Gastrocnemius and or Soleus. Initially, you may not notice the issue, as it starts as a low-level inflammation and micro-tearing, but as the condition progresses, the damage and inflammation become more relevant. Achilles Tendinopathy can be easy to treat and manage when treatment is delivered in the early stages. If the injury is not looked after, the occurring damage could be much harder to resolve. Symptoms Most commonly, people experience pain in the morning or when the muscle is still cold. As the day progress and you start moving around, the pain may dissipate, and you start feeling better, ignoring the danger. Occasionally, the area would present swollen and or tender at the touch. Treatment options for Achilles Tendinopathy The management of this condition starts by improving the rest time and time off from sports activities, such as: Running Soccer Any sport which includes jumping or being on feet Other helpful approaches include: Heat pack Dry needling Improving Ankle and Big toes the mobility Massage Therapy Rock taping Achilles tendinopathies are not a condition that will heal on its own. As mentioned, it will feel better with rest, but as soon extra activities are played, the pain can back as strong as. Remedial Massage and or Myotherapy treatment can help target the painful area, stimulate an immune system response, and help with the recovery process. Also, along with the hands-on deep tissue work, mobilisation is a great way to reduce the tension in the ankle joint and improve the muscles’ functionality. After treatment, Giovanni will give you some exercises to take home. Those exercises would keep the area tension free, improve the joining mobility and strengthen the area.
Tennis elbow or even known as Lateral Epicondylitis, is a condition that occurs on the lateral side of the forearm, at the elbow’s high. A common cause is repetitive motions of the wrist and arm. Tennis Elbow refers to how common this condition can be in tennis players. Said so, Lateral Epicondylitis is a condition that can affect anyone. As per Golfer’s Elbow, the pain starts from the elbow area, in this case from the lateral side, and can irradiate down the arm to the wrist. Rest and counter medication can help relieve symptoms. In some cases, surgery is required. Tennis Elbow Symptoms The pain generated by the tennis elbow may radiate down the forearm along the lateral side (thumb side). In addition to the pain, you may experience weakness too. Here is a list of actions that may be difficult to do Shake hands or grip an object Turn a door handle Hold a cup of water Book now your next appointment to restore the mobility of your Tennis Elbow Causes Tennis Elbow As Lateral Epicondolytis is overuse and strain of muscle, it is caused by repeated contraction of the forearm muscles extensor. These repetitive stretches and movements can lead to tiny tears in the tendon tissue, creating inflammation and pain within the elbow area. Playing tennis with the pour technique often replicates this condition, especially using repeated backhand strokes. Many other common motions can cause tennis elbow. Here is an extended list: Using plumbing tools, which require strong grips Painting Using screwdrivers Food preparation, especially when the knife is not sharp Working in the office using a mouse for long hours Treatment Options At Melbourne Massage and Treatment, Giovanni offers a variety of options for treating Lateral Epicondylitis. MLD may be the most recommended per inflammation of tendons and muscles. Thanks to the light touch and repetitive movement, MLD stimulates the Lymphatic System directly, which takes care of the inflamed area. Combining Myotherapy, Remedial Massage or Thai Massage technique with MLD can help even release more tension along the arm and elbow. Tennis Elbow Exercises In addition to the massage technique offered at Melbourne Massage and Treatment, exercises placed as per usual a crucial role in recovery. Specifically, we can look in too eccentric exercises, which slow, lengthening muscle contractions. Here is a link to eccentric exercises for the Tennis Elbow. As you may notice in this video, the extension motion of the wrist is supported by the other hand. By doing so, the extensor muscle of the forearm that needs training is not working hard. So the actual strengthening happens in the wrist’s flexion when the extensor muscles are stretching under the extra pressure of the weight.