When the lymphatic system stop working, either because for a congential malfunctioning, or because of a an external intervention, which did lead to lymphatic system damage, the individual may start experiencing symptoms of Lymphoedema. At Melbourne Massage and Treatment in Fitzroy North, Giovanni understand how challenging lymphoedema can be, which is why he provide expert care through Manual Lymphatic Drainage (MLD) and Combined Decongestive Therapy (CDT). These non-invasive treatments help manage the symptoms and improve your quality of life. What is Lymphoedema? Lymphoedema occurs when the lymphatic system is blocked or malfunctioning, leading to a buildup of lymphatic fluid. This fluid results in swelling in the affected areas, often in the arms, legs, or other extremities. Lymphoedema can be primary (a hereditary condition) or secondary (often caused by injury, surgery, or infection). The fluid that builds up in the body is a fluid that is naturally produced by the body and is released under the skin and between tissues by the bloodstream. It is reached in protein, bacteria, viruses, dust, and other minor substances that the body is unsure how to handle. Stages of Lymphoedema Lymphoedema progresses in stages, with each stage representing the severity of the condition. Recognizing the symptoms early on can help prevent the condition from advancing, so it’s important to be aware of the subtle changes in your body. Stage 0: Latent or Subclinical Stage In this early stage, there are no visible signs or symptoms of lymphoedema, but the lymphatic system may already be compromised. People in Stage 0 may experience a feeling of heaviness, discomfort, or mild swelling, int the limbs affected by this presentation, but these symptoms typically disappear after resting or with limb elevation. The fluid retention is still minimal and may not be noticed by the individual, but it can be detected through careful assessment. Stage 1: Reversible Stage At this stage, swelling is more noticeable, but the skin is still soft, and the swelling can still decrease with limb elevation and movement. When the swelling is present, the skin will feel puffy or tight, and there may be a sensation of heaviness in the affected area. In this relevant early stage, it i still easy to intervene for prevent further degeneration, and if you are unsure of what you are experiencing, reach out Giovanni for a 15 minutes free consultation, in which, at least thanks to the analysis of your clinical history, we can already evaluate if what you are experiencing is a Stage 1 Lymphoedema. Stage 2: Spontaneously Irreversible Stage In Stage 2, the swelling becomes more persistent and is not fully responsive to movement and limb elevation. The asking of the affected area may begin to feel firmer, and there can be noticeable thickening of the skin. This is the stage where fibrosis (scarring of the tissue) starts to develop, and it’s crucial to stop this from going any worse. While the swelling might fluctuate, it becomes more difficult to manage without intervention. At this point, manual treatments like Manual Lymphatic Drainage (MLD) can significantly help reduce swelling and improve the overall function of the lymphatic system. Stage 3: Lymphostatic Elephantiasis The final stage of lymphoedema is characterized by extreme swelling and thickened, hardened skin. The affected area may look large, disfigured, and become painful to the touch. Tissue fibrosis is advanced, and the skin may develop ulcerations or infections due to poor circulation and immune system function. Indeed, along with the swelling and the fibrosis buildup, the outer layer of the skin is placed further away from the blood capillary, which is responsible for releasing oxygen and other substances essential for skin regeneration.Therefore, as the skin breaks open, due to its poor condition, it is more subject to infections and contamination of pathogens. Stage 3 lymphoedema is debilitating and requires ongoing care and treatment to prevent complications and manage symptoms. At this stage, a combination of therapies such as Combined Decongestive Therapy (CDT) and MLD becomes vital for managing the swelling and restoring lymphatic flow. Common Symptoms of Lymphoedema Lymphoedema symptoms can vary from person to person and depend on the stage of the condition. The common symptoms include: Swelling: The most obvious sign of lymphoedema is swelling in the affected area, typically starting in the arms or legs. The swelling is often gradual and may worsen over the course of the day, especially after prolonged standing or sitting. Tightness or Heaviness: Affected limbs may feel heavy or tight, particularly after physical activity or at the end of the day. This sensation is often worse in the early stages and may become more pronounced as the condition progresses. Pain or Discomfort: Pain, tenderness, or discomfort in the swollen area is common, especially when there is fibrosis (hardening) of the tissues. The pain can range from mild to severe, depending on the stage. Reduced Range of Motion: As the swelling and fibrosis increase, it can lead to a limited range of motion, particularly in the arms and legs. This can impact daily activities and mobility. Skin Changes: In later stages of lymphoedema, the skin may appear thickened or leathery, with a shiny, tight appearance. There may also be visible folds in the skin, particularly around the knees, elbows, or ankles. Frequent Infections: Swollen tissues have a reduced ability to fight off infections, so people with lymphoedema are more susceptible to bacterial and fungal infections, which can further complicate the condition. Numbness or Tingling: As the swelling progresses, the nerves in the affected area may be compressed, leading to sensations of tingling, numbness, or even burning. Increased Skin Sensitivity: The skin in the affected area may become more sensitive, prone to rashes, or develop sores due to the increased swelling and poor circulation. Commonly Affected Areas of the Body Lymphoedema can affect different parts of the body, but the most common areas are: Arms: After surgery, particularly mastectomy (breast cancer surgery) that involves the removal of lymph nodes, the arms are a common site for lymphoedema. The swelling […]
Tag Archives: womanhelath
A surgery is an invasive procedure that involves cutting your skin open to intervene on your musculoskeletal system and or the organs. Surgeries are often a life-saving intervention, but even a life-changing intervention. Once you undergo surgery, your body will never be the same. MLD post-surgery can help stimulate your Lymphatic System, supporting your recovery from this type of intervention. The lymphatic system is a body system that collects, moves and cleans the excess water and substances, like bacteria, viruses, dirt, tattoos, ink and more, from below the skin and then passes it to the bloodstream. Lymphatic System and Surgery. 80% of the Lymphatic System sits below the skin, and 20% sits within the deep fascia. When going for surgery and the skin gets cut, the superficial layer of the lymphatic system gets interrupted and is damaged. Unless we intervene, the lymphatic system will have a hard time regenerating. Indeed, the lymphatic system can regenerate if stimulated. The stimulation of the lymphatic system happens through touch, like with MLD or through the movement of the body, like exercises, even as simple as muscle contraction. MLD Post-Surgery – How It Works? Before or after surgery, it is recommended to stay active. This would allow the different body systems to keep working and maintain their function at their best till the time of the surgery. On the other hand, being active post-surgery is not always an option. In fact, during the post-surgery period, being active in the area that got stitches can be a contraindication, as the stitches could break. A cast may be present in other cases, and the muscle near the surgery can’t be moved. That’s where MLD can help stimulate the lymphatic system. By doing so, we can guarantee the circulation of liquids in the body, which is essential for a great recovery. But not only that Reducing the swelling around the cutting area or below the area affected by the operation would guarantee a fast return to movement. This is because the less swelling, the easier it is to move the joint. But also, MLD comes with a deep relaxation effect, which would put you in a state of relaxation and would help you move more easily. So MLD, by boosting the lymphatic system, reduces the swelling and allows the body’s natural healing process. What to do if you have to go for surgery then? If you are up for surgery soon and you have no contraindication to MLD, what you can do to guarantee a faster recovery is, keep moving as much as you can, stay active, and book yourself in for a few MLD treatments just for the days before your surgery is due. That would help with the Lymphatic System recovery, as a more robust and healthier Lymphatic System would recover faster. And as the risk of infection and post-surgery is under control, and your blood pressure is within the acceptable range (this depends on what type of surgery you had), get moving as much as possible and come back for a few more sessions of MLD. MLD post-Surgery – Does It Work For Any Surgery? C-section (preeclampsia) bone fracture liposuction carpal tunnel knee reconstruction hip replacement day hospital intervention MLD Post-Surgery – What You Should Know As often happens with cancer surgery, lymph nodes get removed if they are contaminated by cancerous cells. After surgery, you may also be treated with chemotherapy or radiotherapy in the area affected by the surgery. Lymph node removal prevents the cancer cells from spreading throughout the rest of the body, so it is often an inevitable step in this type of intervention. The risk of developing lymph node removal, on the other hand, is represented by the development of Lymphoedema after a cancer surgery, which depends on many different factors, including lifestyle, genetics, radiation therapy and more. I dedicated a series of blogs to the Lymphoedema topic, which you can find here. On the other hand, If you are concerned about Lymphoedema presentation, get in touch now to discuss how Giovanni can assist you. Giovanni’s Training For MLD I trained for MLD on two separate occasions with the Vodder Academy, whose courses in Australia are offered by Moving Lymph. The first course I did was in 2021, and I trained to work on patients who had an intact lymphatic system. My training was already complete to work with patients who undergo surgery. It was then in 2024 that I took a course for Lymphoedema therapy. This second had a strong focus on conditions where the lymphatic system is interrupted. Either because of a congenital presentation (primary lymphoedema) or because of external intervention (secondary Lymphoedema). FAQ – MLD post-Surgery
A bunion is a bond malformation at the base of the big toes. The leading causes for bunion are: foot stress high foot arch wearing high heels narrow shoes A bunion is often correlated to Osteoarthritis. Osteoarthritis is due to the cartilage degeneration that separates 2 bonds. In this case, the 2 bonds are at the base of the big toes. This result in pain at big toe extension and during walking. Bunion’s Symptoms Visible malformation, like a bump, on the side of the big toes joint; Sharp pain in the thumb; Difficulties in walking; Stiffness; The big toes point laterally towards the other toes Intervention About what to do for a bunion presentation is to get in touch with a podiatrist as soon as possible. Massage therapy is recommended too, but it is a limited tool for helping in fixing the issue. Along with Remedial Massage, Thai Massage, Myotherapy and MLD treatment, what can be done to alleviate the pain is to treat the surrounding structures, such as the plantar of the foot and the metatarsal area. So, can it alleviate bunion pain and or invert the condition? Yes, it is. Today’s blog post is called “Happy Bunion Story”. So, back in Dec. ’21, Steph start having foot pain, due to osteoarthritis. The reasons behind her conditions are: High foot arch Long hour standing up for work (she is an amazing Wedding and Fashion photographer) Wearing high heels (she used to do modelling) The combination of those resulted in a degeneration of big toes cartilage and a bunion forming. As Steph complained about pain in the big toes, I told her what possibly was happening there. Soon after, she visited her GP and got some X-Ray done, and the result was not much of a surprise. After finding out about her new condition, Steph consulted a podiatrist, who suggested starting a daily routine of exercises for her big toes. Resisted big toes flexion (with a rubber band) Wearing spacer in between the toes Toes abduction from a seated position. But this is not all. The podiatrist even told her to wear an insole in her shoes. Furthermore, she was recommended to buy specific shoes that “protect her foot”. I saw the shoes myself, and I can tell you they didn’t look good. They were thick, big, and didn’t look comfortable to wear. Another podiatrist opinion A few months passed, and I went to see Andy, a podiatrist promoting barefoot wear for my own flat feet condition. As I was talking to Andy about my feet, I couldn’t resist getting an opinion in regard to what Steph was going through. Andy, without much hesitation, suggested that she wear barefoot shoes and continue the exercises. Next, we went down to Sole Mechanic, in Hampton, a shoe shop specialising in barefoot wear. Beforehand we researched different brands and decided to give a goal to the barefoot shoes, “Vivo Barefoot”. Sole Mechanic Experience The experience at Sole Mechanic was a positive one. We booked an appointment for 2 of us, 1 hour all up, so the staff has enough time to guide you through what barefoot is about and the best option. We went through the ankle and toes Range Of Motion and barometric platform test and tried a couple of shoes each. Vivobarefoot, given its ethical approach to shoe wear, was since the start our choice, and so far, the best option we could go for. At this stage, we have a couple of shoes each from Vivo barefoot, one for everyday wear and one for hiking. Back to the “Happy Bunion Story” So, after all this time, Steph now enjoys walking pain-free. The bunion, thanks to the exercises and to Steph’s determination in practising them daily and the new shoes that have a wider shoe box, is reduced, as the Big Toe is now diverging towards the medial side (away from the other toes). Osteoarthritis is a condition that can’t be fixed. Still, when Steph occasionally feels pain we do an MLD session which can help reduce the inflammation symptoms and help in pain management. Said so, the pain is a rare thing and not a daily issue. Furthermore, Steph is not wearing the insole anymore. As suggested by the Sole Mechanic staff, removing the insole is a process that can be done step by step. So, since Feb ’22 when we bought the first pair of Vivobearfoot shoes, took her approximately 2 to 3 months to abandon the insole, and now it is about three months that she is not using it anymore. Hopefully, this post gives you some hope and insights into what’s happening with bunions. If you are in pain and need to reduce the inflammation response to the bunion, MLD may be best for you as a short-term solution. Otherwise, book an appointment with Andy to find out the best way to adjust the shape of your foot as much as possible.
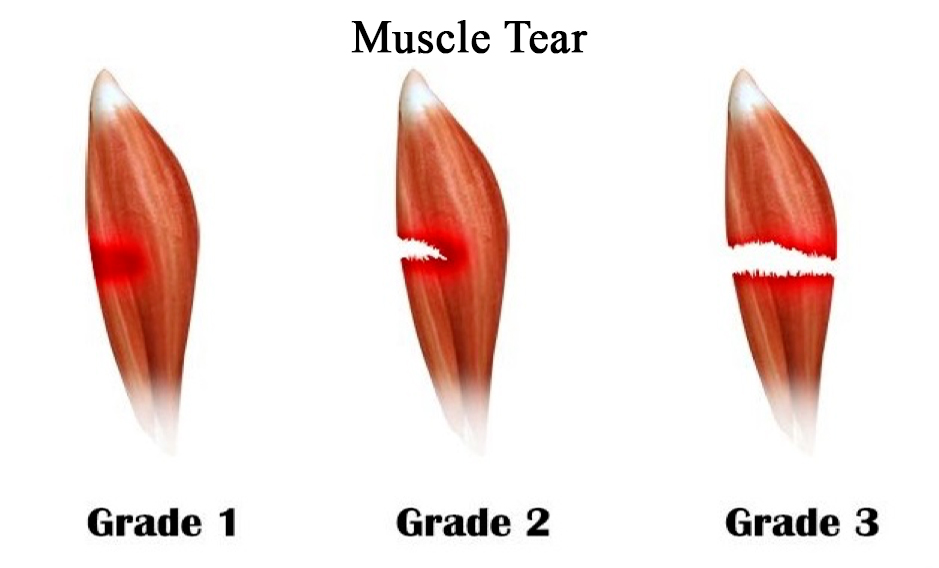
A muscle tear is an acute injury caused by a laceration of the muscle cells/fibres and or tendon to which the muscle is attached to. How can happen a muscle tear? A muscle tear happens when a muscle is weak and don’t activate at the right time. Weak muscles are common in repetitive movement or when a muscle overcompensates due to a fragile pattern. For example, tearing a hamstring is expected when the Gluteal Firing pattern is incorrect. This type of injury is common in sports activities. Still, it can also happen within a home environment by lifting a box incorrectly or during garden activities. The three grades of muscle tear. Grade 1 muscle tear is the mildest one. As per this case, only a few muscle cells have been torn. Symptoms are like: mild pain, moderate swelling, none or light bruising. In grade 2, a moderate amount of muscle cells have been damaged. Symptoms are like: Bruising is now more evident as per the swelling You must luckily hear a sound as the tear happens More severe pain, especially when trying to use that muscle. Grade 3 is the worst-case scenario. In grade 3 muscle tear, the muscle has fully torn. Still, a pop or a sound would happen as the tear happens. On the opposite side of where the muscle did lacerate, you will notice a bulge as the muscle coiled up after tearing. Weakness in using the limb where the muscle got torn. In case of a Grade 3 muscle tear, surgery is needed to reattach the muscle. How to treat a muscle tear? The immediate appliance of heat or cold packs is highly debated. A cold pack would numb the area and help with the pain symptoms. As mentioned in the “Ice Pack” blog post, that is actually recommended. On the other hand, a heat pack would help stimulate blood circulation in the affected area, reduce swelling, and boost recovery. It’s important to note that applying a heat pack too soon after an injury can actually make things worse. It’s best to wait until the acute phase has passed, which typically takes around 48 hours. At that point, heat therapy can be a helpful way to alleviate pain and promote healing. Regarding massage treatments, MLD can be the only technique used as soon as the tear happens. Indeed MLD would be highly recommended for boosting the recovery, especially in case of a tear in 3rd grade, where operation is needed. In case of a 3rd-grade muscle tear, the first thing to do is see a doctor. Other massage techniques, such as Myotherapy, Remedial Massage and Thai Massage, are still valuable for muscle tears. On the other hand, either Myotherapy, Remedial or Thai Massage can only be practised after 48 hours of rest are passed after the incidents. Indeed that 48 h is considered the acute phase of the muscle tear. How to prevent a muscle tear? More the body moves, the less the chance of injury. Making sure to do simple exercises involving basic body movement can help in muscle tear prevention. but not only. Keeping the joint moving is another essential aspect of injury prevention. How can massage help? Along with a massage treatment, the area of focus will be the torn muscle and surrounding area. Initially, the technique used with a massage treatment, especially for the injured area, would be MFTT and passive movement/mobilisation. That would help muscle recovery and facilitate joint mobility, reducing the muscle’s load. Going ahead with the treatments, techniques such as MET, a resisted muscle force technique, can be used. This would allow the muscle to gain elasticity. Book your next session by clicking here if you are suspicious of a muscle tear and need treatment.
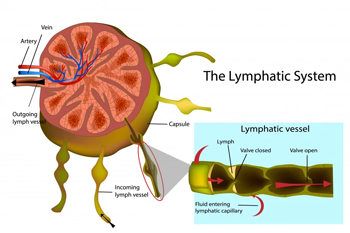
Lymph nodes (or lymph glands) are small lumps of tissue containing white blood cells that fight infection. They are part of the body’s immune system and filter lymph fluid, composed of water and waste products from body tissues. Introduction to Lymph Nodes Lymph nodes are located in different body areas. On average, we have approx 600 LN. In the neck area only, we find 160 LN itself. LN can vary in size and go from 2 to 30 mm. Lymph Nodes are connected by vessels, better known as afferent and efferent vessels. The afferent vessels carry the lymph to the lymph node, and the efferent vessels take the lymph away from the lymph nodes. So, the lymph nodes are also connected directly to the blood system, veins, and arteria. What is a lymph node made of? Despite the structures that enter and leave the lymph node, these cleaning stations are made of: Connective tissue capsule Supporting strands of connective tissue inside Below the marginal sinus, there are clusters of lymphocytes lymphoid follicles Artery, vein and nerve As for the filtering station, the lymph node is essential to ensure that no bacteria, viruses or dirt can access the blood system. Where we find no lymph nodes in the brain. Indeed, the lymph fluid around this area gets drained by the Optic and Olfactory nerve. Following then the position of the lymph nodes, we can define the watershed. MLD and Lymph Nodes. Lymph Nodes can occasionally be swollen, which happens when the body fights an infection. In my practitioner experience, I often have to refer to the lymph node concept to introduce the client to MLD treatment. Not many clients know about this technique; they are more familiar with Myotherapy or Thai Massage and Remedial Massage. Said so, the client who tried MLD are all well impressed with its benefit. During an MLD session, what happens is that with a gentle stretch and recoil of the skin, I help your lymphatic system to work faster. Consequently, that’s how swollen area gets reduced. In pushing your lymphatic system to work harder, the lymph node would receive more liquid to process. On the other hand, knowing where the lymph nodes are, is essential to ensure we push the lymph liquid in the right direction. If you haven’t booked your appointment yet and wish to set a goal for MLD, please follow this link.
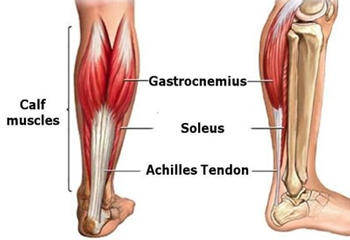
Calf muscles make up the lower posterior portion of the leg. Calf Muscles are: 2 are the calf muscles, the Gastrocnemius and Soleus. Below is a table with Gastrocnemius and Soleus’s Origin, Insertion and Action. Gastrocnemius Origin The posterior surface of the lateral and medial condyle of the femurs Insertion Calcaneus via calcaneus tendon Action Flex the knee Plantar flex the ankle Soleus Origin Soleal line; the proximal posterior surface of the tibia and posterior aspect of the head of the fibula Insertion Action Plantar flex the ankle So, due to their origins and insertions, we can clearly understand how the Gastrocnemius is involved in knee flexion and how the Soleus is not. The Gastrocnemius does across the knee, as it originates from the femur itself. On the other hand, the Soleus doesn’t cross the knee, so it doesn’t play any role at the knee level. This aspect is so important to differentiate what of these 2 muscles are involved in the restrictive movement at the ankle, and or in calf pain. Calf Muscles testing Firstly the patient is lying down in a supine position (face up) doing active dorsiflexion. Secondly, we will ask the patient to lie in a prone position (face down), and we knee bend (passively), they would go in ankle dorsiflexion again. What happens there is when the knee is flexed passively, the Gastrocnemius is deactivated, and so the ankle dorsiflexion is happening by pulling the soleus only. Now, 2 are the case scenarios that could happen: Still a limited range of motion at ankle dorsiflexion with or without pain A better quality of ROM with a greater angle in dorsiflexion. In the first case, the tension muscles could still be both. In the second case, the Gastrocnemius is clearly the muscle limiting the ROM. For ankle ROM in dorsiflexion, we are looking for a minimum of 20° to up to 30°. It is not all about Muscle Pain. But can calf pain be related to something else and not just to muscle pain? The answer is YES. Calf muscle pain can be a RED FLEG for Deep Veins Thrombosis (DVT), especially after a flight. DVT Symptoms: Sharp pain; Heat at the touch; Soreness at the touch; Redness on the skin. In this case, you want to contact your GP immediately. Massages are absolute contraindications. In conclusion, for a full calf or muscle recovery, we want to look in too some exercises. Remedial Massage, Myotherapy, and Thai Massage are great ways to reduce pain and manage symptoms, but exercises are essential actually to heal a muscle. Indeed, when we talked about plantar fasciitis, those exercises are something that we can look at for calf strengthening.
When experiencing pain around the head, we talk about Headaches. Headache is a common condition, and for most cases, is not considered a serious illness. Migraine and headache. 4.9 million Australians experience migraine. Migraine is a specific type of headache, so consider that the number stated above is still a small figure. Headache and muscle. If you ever experience a headache, you may notice that the pain sensation does start from your cervical area. Or, by confronting yourself with who is around you, your headache pain pattern, is consistent, but it is different from the one of someone else. On the other hand, you may associate headaches to the result of a heavy drinking night, or of lack of water (which is why you get headaches after a heavy drinking night, by the way), but often headaches are there because of cervical muscle tightness. Wait, what? Yes, you did read right. How can we define then if the headaches come from muscle tension? So in order for this to happen, the muscle responsible for referring its pain up to the head must be tight or stretched out, and loaded with trigger points. As massage therapists, especially in the first consultation session, we would ask about headaches and if there are any, “where about do you feel the headache”? Indeed, the answer to this question is most luckily the giveaway to know which muscle is may responsible for your headaches. To confirm the suspicions, we would then assess your posture, looking for any muscular-skeletal unbalance, and then we would assess the Range of Motion (ROM). If the ROM show up to be limited on the muscle that we believe is responsible for the pain in the head, then most luckily we are halfway through the solution. I do say halfway through, a single massage session either Myotherapy, Remedial Massage, Thai Massage, or MLD is maybe not enough to release all the tension that is in needs to be alleviated to eradicate the headache. Said so, no journey starts, without doing the first step, isn’t it? When a headache is a Red Flag? For red flags, we refer to symptoms that may be present due to serious illness or condition. Some example includes clients who had a clinical history of stroke and or brain cancer, a recent car accident or recent head trauma, or blurred vision. If that’s the case, the next step is referring the client to a GP immediately for further investigation. What about the cervical muscle tension headaches type of presentation? As already mentioned in another blog post, the Occipital muscle can have headache type of pain in the lower section of the posterior side of the skull. If we then look into the area of the skull that seat above the ear, could be more tension from the Upper trap or Levator Scapulae. By keep moving more medially and above the head, Splenius cervis can refer to the medial superior side of the head and Splenius capitis to the middle top side of the head. Sternocleidomastoid, indeed, can refer to the frontal lobe of the skull. Now, all these muscles are sitting on the neck and throat and from above the shoulder. So, ensuring that those areas are free or not overloaded with tension can help in staying headache-free. Now, in this blog post, we are keeping the headache presentation type of pain to its simple aspects. On the other hand, the topic can be further discussed in person with Giovanni during your next massage appointment. Book now your next massage session, if you are trying to get to sort out your headache presentation. Other approaches to a headache-free life, out of massage therapy. There is a series of things that complimentary massage can help with to relieve headache pain. Exercises Keep yourself hydrated Good posture when seating and standing Good variety of food as diet intake Wearing glasses if needed. Meditation for stress management In conclusion, headache is a really common problem for all Australians, for both women and men. Don’t wait for your symptoms to get worse; you may not need to take medicine all the time if you have a headache, as the medicine will just numb the symptom but will not sort out the problem. If you are keen to learn more about where your headache may be coming from, book your next Massage Session today.
Water after a massage. Have you ever noticed that after a massage you feel thirsty and depending on the treatment you may have an urgency to go to the toilet? Well, massages are diuretics, that’s why. Indeed, independently of the type of treatment that you receive, whether is MLD, Remedial Massage, or Thai Massage, the body fluid gets pushed and pumped around the all body. As per consequence, all these substances moved around need to find their way out. So, after any session, you wanna make sure to rehydrate your body. Drink water after a massage. Why water and not orange juice? Or an energy drink? Or coffee? Water is what is recommended after a massage because it’s what can at the best re-oxygenate the muscle and re-hydrate the body. Drinking a sugary drink, or a really acid beverage as it can be coffee will just dry off the body even more. Furthermore, water is quicker to be absorbed and can help the stomach to keep its natural PH balance. If this post is talking to you, book your next massage session by clicking here. Another effect of the massage can be the deep relaxation of the body, which can affect the stomach and abdominal feeling. Indeed, adding sugar or other substances to the PH of a stomach that feels so relaxed, may not work at the best. What about the water temperature then? Cold or warm? Well, let’s take down the myth that cold water makes you feel fresher. Sorry, it doesn’t. Drinking cold water brings the body temperature down, increasing then the difference in temperature between within the body and outside the body. That will make you feel even hotter. But I do understand that hot water unless is herbal tea, doesn’t feel so nice. Even though, warm water would be ideal, as its temperature would be the same as one of our inner organs. So, temperature-wise just drinks water at room temperature if you can’t stand hot water.
Quietly often I still get asked what is cupping and how does cupping work? Firstly, Cupping is a type of alternative therapy based on placing cups on the skin to create suction. Indeed, the suction would pull the skin up from the muscle layer, drugging back the fascia layer seating below it. Cupping is gentle work on the body, not invasive and at the same time is an amazing technique to stimulate and facilitate the fascia. We did look into the fascia in a previous blog post. If you have missed it, you may wanna click here. On the other hand, there are different types of beliefs and methodologies about cupping’s functionality. Some of those can be a bit more invasive, and dangerous too. Said so, I guarantee my clients that these are not practices that are available at Melbourne Massage and Treatment. For how I got trained in giving cupping, my aiming as giving cupping is: – Leave no marks – No cutting the skin – Painfree – No blood stagnation Now, by following the order of the action listed here above: Marks are a sign of blood stagnation. Accidentally can happen to leave a mark on someone’s skin, and many are factors involved in it: Skin type is one and another one is if the area that received cup was already massaged or not. As Remedial Massage therapists or Thai Massage Therapists, we are NOT trained to cut anyone’s skin. Furthermore, you have to think that when this practice is involved there is a great risk of skin infection. Why do some practitioners do so?! None of my business. I just don’t believe it is necessary, and I don’t believe it has any benefit. As per many detox diets and detox programs, the body is your best allay and best detoxer of itself. If this post is talking to you, and you are in need of a massage, book your next session by clicking here. In regards to pain, Cupping must be pain-free. Along a cupping session, you may feel a strong pull along the skin, but no sharp, ache or pinch sensation should be present at any moment. Indeed, to help the cup slide easily oil or cream oil-based get used. When happens that a mark gets left behind, doesn’t necessarily create pain or discomfort. Another cupping precaution is to avoid over-pass a cup on joints and or tendons. The cupping force could rip or damage those areas, resulting in permanent damage and pain. Lastly, no blood stagnation. Cupping’s desired result as per many massage modalities is to generate a physiological response that would reduce tissue stress. Through the gentle tissue stress, muscles relaxed and the chain of manual therapy benefits starts.
Manual Lymphatic Drainage if used along the correct type of condition, is a safe and well utile manual therapy. In the previous two blogs (Link 1, Link 2) I described how the Lymphatic System works and its relation to MLD. What body find benefit from Manual Lymphatic Drainage? As previously mentioned, the lymphatic system is so important to keep the homoeostasis of the body. Indeed, along with the following conditions, homoeostasis is compromised: Skin Burn Chronic Inflammation (plantar fascitis, tendinitis…) Lymphodema Oedema Scar reduction and prevention Pre and post-operation body rehabilitation Improving the bell function Head-each Skin puffiness and or Acne and more… How can Manual Lymphatic Drainage help with these conditions? Firstly, what all those conditions have in common, is that they are related to how the Lymphatic System deal with them. So again, the healthier and more vital is the lymphatic system, the better the body’s homoeostasis. If we look into oedema due to a hammered hand, we need a responsive and well-functioning lymphatic system to absorb that swelling. The stronger the lymphatic system, the quicker the healing process will be. Even a scar from a post-operation could heal faster if the lymphatic system gets adequately stimulated. More nutrients and less dangerous components will float around the wound if the lymphatic system works stronger. Secondly, some of these conditions are so painful that a massage is not applicable. As we applied MLD, we would not increase the pain, thanks to the light touch. If this post is talking to you, and you need a massage, book your next session by clicking here. Why should MLD not be painful? When we apply the different strokes by dragging the skin gently around, we will stimulate the lymph vessels to collect the obligatory lymph load. Still, we will not generate pain by stimulating pain receptors. Furthermore, the repetitive mechanical stimulation would activate what in science is called the gate theory. The gate theory looks into the interneurons’ inhibitory response, which reduces the pain signal reaching the brain, consequently decreasing the pain response. MLD and coontroindications. MLD can’t be applied to Acute infection, Untreated Cancers, Untreated Thrombus, Congestive heart failure, or intoxicated persons. Minor contraindications include Hypertension/Diabetes n1, Autoimmune disease, Asthma, Hypo/Hyperthyroidism, pregnancy, and a history of tuberculosis. In conclusion, I am honoured to have the knowledge and the skill to use and apply such a technique. Even though, for now, I can’t yet treat people with Lymphodema and or clients who had lymph nodes removed or are looking for a post-cancer treatment. What I got to offer to this patient, anyway, is a reference for other practitioners. So if this is you, please get in touch with me, and I can refer you to your nearest practitioner.
- 1
- 2