Plantar Fasciitis is a foot condition that can cause severe pain when walking or standing. Pain may be more intense in the morning when you step out of bed. If you ever had plantar fasciitis you will well know, that is not a fun thing to deal with. How to fix plantar fasciitis? In most cases, corrective exercises are the best way to retrain the foot and heal it once and for all from this condition. In this blog post, I talk more in detail about exercises for plantar fasciitis. How does Plantar Fasciitis manifest itself? Plantar Fasciitis manifest itself when the load of the foot is predominately put on the outside of the foot or on the back of the foot. It is the case we talk about an over-inverted foot, indeed a foot that is overloaded on its lateral portion. By doing so, the big toes flexor, the muscles that connect the big toes to the heel, get inflamed. As per consequence, pain does manifest below the heel. “It feels like if I got glass under my feet” someone that offers this condition would say. Plantar fasciitis demographic. People who spend a long time standing up/walking (waiters) Runners (who run with a heel strike) Pregnant women (due to the abundance of weight) The foot is a complex body part. Indeed, the foot contains 29 muscles, 26 bones and 30 joints. Therefore if not loaded correctly, the consequence can lead to major body musculoskeletal dysfunctions and unbalance. As already mentioned during the blog about the Fascia line, unbalanced feet can reproduce tension up to the back and shoulders. Plantar fasciitis functional test. A simple test that we do as massage therapists is to passively extend the big toes. (Windlass Test) If pain is reproduced on the heel, the test is positive. Therefore, this test tells us that the big toes, which most luckily would not even extend to their full range (65°), are not used when standing and or walking. That’s why is weak and tight. How can massage help reduce plantar fasciitis pain? At Melbourne Massage and Treatment, Myotherapy, Remedial Massage or Thai Massage can help reduce the tension along with the foot’s supinator muscles, which are responsible for over-invert the foot. That’s one of the reasons why the body weight gets overloaded on the lateral side of the foot. Regarding MLD, it can be most beneficial to reduce the inflammation within the plantar of the foot and help manage the pain. But as previously mentioned, massage can help in reducing the symptoms, and improve mobility. Where for full recovery, corrective exercises are essential. Was this post helpful? If you are suffering from Plantar Fascitis and would like to find a way out of the pain, book now your next appointment with Melbourne Thai Treatment. Here on the right side, is an example of a pair of shoes, for someone who suffers from plantar fasciitis. As you may notice, the lateral portion of the show is completely worn out, where the medial portion, is nearly touched, especially at the big toes area. So back to the fact, that the big toes are what should drive the foot along the strike motion if that shoe area is untouched, it means that person is not loading any weight on there. Footwear examination can be also used to identify weight balance in the foot area.
Monthly Archives: April 2022
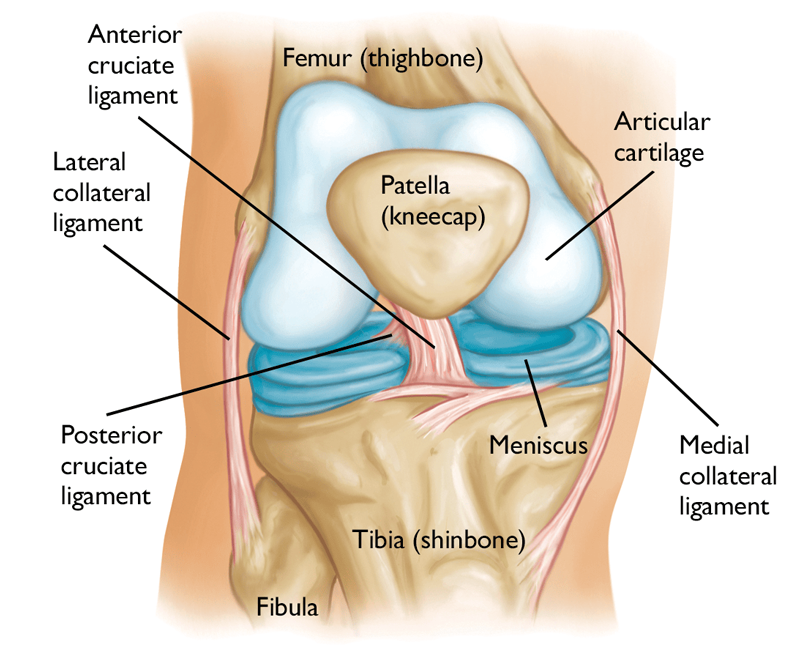
Knee pain is a common presentation for clients of any range of age and gender. Knee pain indeed is a vast topic. So in this post, we are going to go through how to identify the reason why we can experience knee pain. For doing so we are going to look at some special testing, that we use for the knee joints. Next, in a further post, we may analyse individual conditions. What about the Knee Joint? The knee is the strongest joint in the body. It takes a lot of pressure from the upper body and still has to handle the shock coming from the lower leg session, shock as walking, running and jumping. Indeed, whenever we do one of these actions, the knee plays a big role. Knee Anatomy Bond: Above: Femur Below: Medially the Tibia, laterally the Fibula. Patellar is the front “floating bond” Ligaments: Anterior Crucial Ligament Posterior Crucial Ligament Posterior Menisco-Femoral Ligament Fibular Collateral Ligament Tibial Collateral Ligament Transverse Ligament (this one is visible only from the front side of the knee, below the patella). In between the bonds we have: Medial Meniscus Lateral Meniscus If this post is talking to you, book your next massage session by clicking here. So, the knee joint can be divided into two parts: Tibiofemoral joint Connects through the collateral ligaments, cruciate ligaments and menisci; Patellofemoral joint Gives stability to the medial and lateral retinaculum and allows the extension mechanism through the tendons of the quadriceps f.. Now that we have a better idea of what the knee anatomy is, we can look into his functionality. Knee ROM are: Extension: 0° Flexion: 140° Internal Rotation: 30° External Rotation: 40° Abduction/Adduction: 15° Said so, we can see that the major movement that the knee can accomplish is, flexion. Even if the Internal and External rotation since to be a big move for the knee, in the reality, that’s not always the case. The older we get, easily this motion actively gets tighter. Indeed, one of the main reason for meniscus injury is the twisting of the knee, when the feet is holding the ground and the body rotates. But as previously mentioned in this post we would look into the knee special test. What knee functional test have to tell us? As we already mentioned in another post, a generic active, passive or resisted ROM tell us about muscle functionality. On the other hand, a special test for the knee can show us if a ligament or a meniscus is loose, in the case of ligament or injured. Furthermore, special tests, on the knee are essential to prevent further injury and reduce joint degeneration. To start with we have the drawer test: Anterior Draw test and Posterior Draw test. The Anterior one is to test the anterior crucial ligament, and the posterior, obviously, is for the crucial posterior ligament. Both these tests are done with the client lying supine on the table, with a hip and knee flexed, and foot on the table. The therapist will ensure that the foot doesn’t move and will place its hands around the knee, with the fingers (except the thumb) seating at the top of the calf and the thumbs seating on the patella. For the A.D. test, the therapist will lightly pull the knee joint away from the patient body. On the other hand, for the P.D. test, the therapist will push the knee towards the patient’s body. These tests are positive if there is a loose movement within the knee, in the direction of pull or push. If the client has a history of injuries, to the ACL or PCL the therapist wants to make sure not to push or pull with great effort, or injury could occur. Vagus and varus test. Those tests analyse the status of the medial and lateral ligaments. For the valgus test, the therapist places one hand above the knee laterally, and the other hand above the ankle on the medial side. By applying opposite pressure in the 2 directions we put the medial ligament under stress. If pain is reproduced, or there is a loose movement the test is positive. The same action is for the Varus test. In this case, the hands are placed still above the knee and ankle, but the bottom hand is placed laterally and the top one, is placed medially. Apleys Test This test is used to evaluate the state of the meniscus. The client, in this case, would be lying in a prone position, with the knee flexed. The therapist will be standing next to the client, on the side of the knee flexed and will apply pressure to the knee. If no pain is reproduced with pressure only, the therapist can gently apply a rotation movement to the flexed knee. The test is positive if the pain is reproduced. McMurray test. This is luckily the most efficient and most used knee test used by therapists in case of meniscus injury Here is how it works: The patient lies in the supine position with the knee completely flexed (heel to glute). Lateral Meniscus: the examiner then medially rotates the tibia and extends the knee. Medial Meniscus: the examiner then laterally rotates the tibia and extends the knee. McMurray is a positive test if the pain is reproduced. There are still a couple of tests that can be done for the knee, but so far we did cover the most important. About the therapy that I can offer for releasing knee pain, MLD is what I would suggest the most. Especially for acute pain and swelling or oedema reduction. Whereas, Myotherapy or Remedial Massage and Thai Massage can be used too but more to facilitate and or strengthen the muscle surrounding the area.
A Scap-Off Load is a special test or functional test that we use to evaluate the implication of Lev Scapular and Up. Trap in Cercival Rotation. As previously mentioned, in cervical rotation, we got a fair bit of muscle working towards this action. As many clients come in with cervical pain, it’s time to explain in more detail what’s going on there. Cervical Rotation. How does it happen? So, when we rotate our head, either right or left, the muscle on the same side of the rotation movement is contracting. If a muscle along those is weak, we may reproduce pain in rotation along the same side. To thin down which muscle is responsible for the limited ROM, we have to safely deactivate some of them to see if the left behind one can deliver the expected movement. Here is an example of how scap offload works. If a client comes in with 30° Cervical rotation on the R and pain on top of the scapula, that could be an indication that its levator scapulae is the muscle to target. To confirm this hypothesis, I would ask the client to shrug their shoulders and flex their elbow (the client is sitting on a stool). After that, I will make my way behind the client, and I will support their shoulder weight with my forearm and hands. As the client relieves the shoulder tension, that lev scapulae and up. Traps. are now deactivated. The next thing would be to ask the client to perform the cervical rotation. Ideally, I would like to see the client have a full range of motion (80° to 90°). If this post talks to you, book your next massage session by clicking here. That would tell me that the only muscles that are limiting the cervical rotation are the lev scap. and up trap. On the other hand, what could happen, is that the cervical rotation is, yes improved, but still limited, compared to the ROM expected. In this case, the muscles involved in the stiff range of motions are not only lev scap. and or upper trap. In fact, what is causing the limitation is the cervical occipital muscles. And yes, spending long hours at the computer or looking at the phone doesn’t help. After this test, to narrow down even more which other muscles are involved in the stiffness of the cervical area, I do run another series of tests. Those tests would look into joint areas like C0-C1, which would refer to Obliquus Capitis Superior muscle, and the C1-C2 test, which would look at tension for Obliquus Capitis Inferior. Furthermore, for the other facet joints that make up the lower cervical region (C3 to C8), I would analyze each facet joint individually. These series of tests are indeed part of my Myotherapy training. Last would be then the usage of the joint mobilisation technique. In this case, we would look into what joint has lost mobility or which one has an excess of it. Strengthening the cervical. In order to improve the presentation, massage on its own is not enough. As per any condition so far, the strengthening of the muscle, in this case, the cervical and upper thoracic one, would allow to prevent further pain and discomfort. The work that the cervical muscle has to do daily is considerably high, giving the natural weight of the skull. So exercising a chin tag in a supine position can help. Ideally, we would do these exercises in the supine position (lying down face up) so that we have gravity to fight back as we train our deep flexors. To further improve the strengthening, once the chin tag is not enough, we can start using a soft rubber band to create resistance. Said so, be mindful that the cervical area is a delicate area to work on too, and those exercises are best practice under the supervision of an expert trainer or massage therapist.
First Massage Appointment. At Melbourne Thai Treatment, a first massage appointment session does last a bit longer than a regular appointment. Indeed, if you go on the booking page, you may notice that the first appointment lasted 75mins. Why so?! Well, within the first appointment, as a therapist my aim is to track down your Clinical History. For doing so there is initially a form to fill in and in a second stage few subjective questions that I am going to ask. Questions are like: “What do you do for work?” “What sports activity do you do or did?” “On what side do you sleep?” “Are you Right or Left Handed?” Ext… These and other questions, relevant always to the presentation that you come in with, are for me therapist essential to understand how you end up having the pain or discomfort that I have to remove or reduce. Obviously, those questions asked during the first massage appointment can take a bit of time to be answered Occasionally an answer gives space to a new question. Said so, the more specific are the answer more I can narrow down the clinical situation. If this post is talking to you, book your next massage session by clicking here. As per result, will be easier to find a path to alleviate pain and discomfort. On the other hand, as the session last longer than a regular visit, as a therapist I charge a bit more. For a Remedial Massage and a Thai Massage a first appointment session would last 75mins. About MLD a first Massage session would last 60 minutes. Indeed, with this post, I would like to share and explain to any clients that the first appointment is not more expensive because I am greedy. Is through, the time we spend doing the massage itself is per usual the same time that we would spend during a general consultation. But, that initial time that we spend working out your Clinical History, will save time after actually treating the condition. In conclusion, I would not see the first appointment as an extra expense, but as an investment in your health. Before we find out what’s the cause of your pain, and discomfort before I can create a proper treatment for it.