A pain response is a signal created by the brain to let you know that something within the body is not right, or at least, that something, potentially, is not right. This means that pain is a sensation that can also be there when no actual damage is present in the first place. But when you feel pain in the neck, in the shoulder, in the knee or somewhere, how can you differentiate if it is a pain given by muscles or by a joint? In this blog, I want to talk about the difference between muscle pain and joint pain.
Muscle and Joint Pain: Let’s Start With Clinical History Intake
When someone presents to the clinic in pain, the first thing I do is to track down their medical history, which includes their daily activities, previous injuries (old and recent), sports history, medications, quality of sleep, etc.. From there, I start to narrow down when they have been experiencing the pain, and what caused it in the first place, and where they feel it. Already, that information can give a good perspective of what we are looking at, in terms of muscle pain and joint pain.
Knowing the time frame of the pain, the location of the pain can already give an answer. But before jumping to conclusions, we need to do some testing
Active and Passive Movement: The Differences In Pain Response
After an accurate intake of the clinical history, we would proceed with some testing, including active and passive range of motions.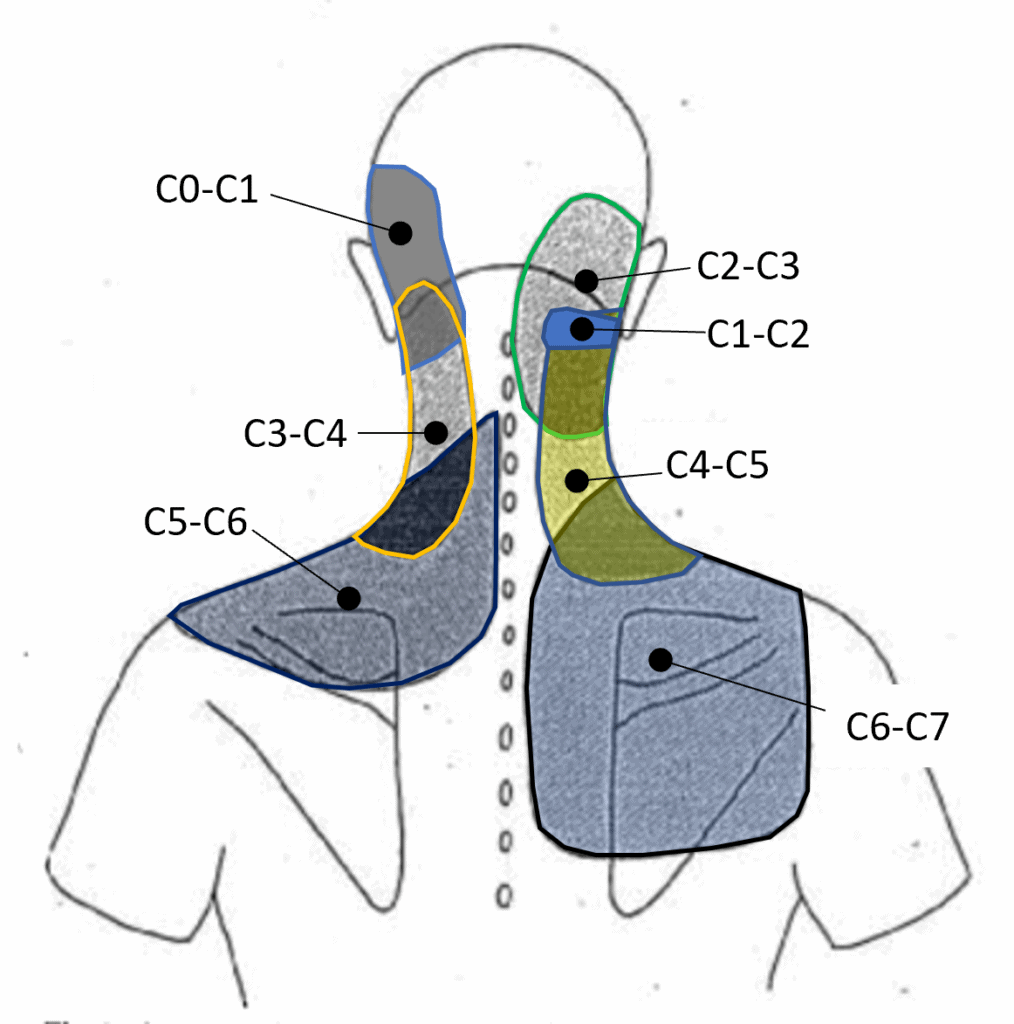
Active range of motions (AROM) are those movements that the patient would do on their own, like flexing the shoulder, rotating the hip, etc Passive range of motions (PROM), on the other hand, are movements that the therapist would do with the patient’s body. So you will be asked to keep your arm and shoulder relaxed, and it will be the therapist who moves the arm.
Here is where things start to get interesting.
If you respond with pain with AROM, we know that you are using both your muscle and joint to deliver the movement, so the pain response that you feel could be either from the muscle or the joint.
But if you respond with pain with a PROM, then we know that the response is from the joint, because the muscle, in that specific motion, is not working.
How about tendon?
So, when delivering a PROM, we may push the movement to its limit, creating a stretch motion.
This specific endpoint of movement, if it reproduces a really pinpoint specific pain, that is sitting right on to what we can recall as a tendon (the insertion point of the muscle), it is another differential tool to understand what the pain is caused by.
So yes, to simplify, we use PROM to identify a joint pain, but in that joint pain, we include the tendon itself, not only the ligaments.
Ligaments, per clarification, are the tissues that hold the bones together and make up the joint.
Orthopedic testing: another tool for differentiating muscle pain from joint pain
But the rabbit hole of understanding where that pain is from doesn’t stop here.
That’s why we also use orthopedic testing when looking at a pain presentation. Ortopedic testing is a test that places stress on a specific structure, and can have a range of sensitivity and specificity.
- Sensitivity refers to the test’s ability to identify individuals who have the condition being tested for.
- Specificity refers to its ability to identify individuals who do not have the condition.
Those two terms, that get evaluated in %, can tell us how valuable a test is. And most often, to validate a hypothesis of what can cause the pain, we have to use multiple forms of testing, from AROM to PROM to orthopedic testing and Clinical History.
Neck Pain: Muscle Pain or Joint Pain – A case study
Neck or upper shoulder pain is one of those common presentations, where the patient presents thinking that it is due to a muscle issue, but then, you prove to them that it is actually their joint that is the issue.
Who is Peter, and with what pain does he present himself?
Let’s examine a case study of Peter (name of fantasy), a 43-year-old office worker presenting with pain radiating from his right neck to the upper shoulder. Despite various stretches, the pain persists. He tried many pillows, he tried any sleep position, but this pain comes and goes, and has been on for years.
Peter presents with a pain level today of 7/10, complaining that certain neck movements are limited and painful. It is hard, for example, to do a head check while driving.
Clinical History
So, first thing I would do is go through Peter’s clinical history and find out that his pain started about 10 years ago, after a whiplash accident, and that at that time, more than having a collar on his neck for a week or two, he hadn’t done much about it. Hi pain, which occasionally radiates to the neck, also gives him a headache. Sport history includes playing AFL from when he was a kid till his mid-twenties, and nowadays the occasional swim, yoga and pilates class. He spends most of his days working from home or at the office, sitting in a chair.
In addition to this, we also know that:
- No pain radiating down the arms, no pins and needles in the hands;
- Pain is worst in the morning;
- Stretching gives an initial relief, but then it gets worse.
Differential Diagnoses (DD)
Differential diagnoses are the hypotheses we think of when someone presents with pain.
Let’s say that is what we think we could find as a problem, given the patient’s complaint we received. And out of 3 or 4 DD’s, we will draw a line that connects all the results and get a Working Diagnosis (WD), which is the most plausible answer given the results we obtained.
This said, this is not an official diagnosis, which can be used at a medical level to justify the pain. But it is a step-by-step reasoning that allows us, manual therapists, to justify why we would use certain hands-on treatment and give certain exercises to improve the presentation.
DD1: wreck neck
DD2: Cervical Facet Joint sub-acute irritation
DD3: Nerve entrapment along the cervical joint
Testing
AROM
Starting with AROM, of his cervical area (neck) Peter has pain in his right neck when rotating to the R, and when he rotates to the left, he feels his neck is stuck, but not much pain in there. Other AROM, like extension, is painful, and flexion is limited. Lateral flex to the R is really limited and painful, and to the L only limited (he feels the R side being blocked when he laterally flexes to the L).
When complaining of pain on his right side, he also mentioned that the pain is felt in the neck and down to the right shoulder, in a broad area.
Along with AROM, we also test other joints, like the shoulder and the thoracic. And we do this to see what’s going on along the mobility stability joint line.
This results in no abduction detected at the shoulder level, but a lack of mobility in thoracic rotation and lateral flexion.
Orthopedic Test
Before proceeding with PROM, I apply a test call scap off load, which is an orthopedic test, where the patient gets asked to stay seated and perform cervical rotation, while I hold their shoulder shrugged up. The result of this test, for Peter, is negative, which means, yes, he can move a bit more but he still feel the pain. So even though the muscles connecting the cervical to the scapula are shrunk and hanging there, Peter still experiences pain.
PROM
To deliver a passive range of motion for the neck, I will ask Peter to lie down on the table in a supine position, and from that position, I will stand behind his head, and with my hands, I will take his neck in a specific PROM with gentle and controlled motions. So far, I will apply three types of movements for each side:
- Lat flex at C0/C1 level;
- Full flexion of the head, with rotation – R & L – this is to see a response from C1/C2 level;
- In a rested position, I will fully rotate the head to the R & L – this is to see a response from C3/C7.
While doing the PROM, Peter responded with pain while I flexed his head forward and rotated to the R (C1/C2), and he also responded with pain while I rotated the head to either the R or L, but the pain was always on the R side, and it did radiate to the shoulder.
Passive Accessory Intervertebral Movement (PAIVM)
PAIVM are a series of PROM applied to the spine to identify any painful response at the joint movement, or the level of stiffness that the joint presents with. In Peter’s case, the right side of his neck responds with a high pain response (7/10) specifically when working on the cervical level between C2 and C7.
Working Diagnosis (WD)
Given the result from the testing and a summary of the clinical history, I would be suspicious that Peter suffers from:
- a sub-acute facet joint irritation which started post car accident (whiplash), maintained by lack of thoracic mobility, and cervical muscle strength (he never worked on it).
Why do I consider this to be Joint Pain and not Muscle Pain?
What made me conclude that this painful presentation is due to joint and not muscle is due to:
- No recent mechanism of injury – muscle healing time is quick, we talk about 8 to 12 weeks, even if you have a bad muscle tear. Peter has been in pain for 10 years.
- Pain is exhibited when doing PROM and PAIVM – as mentioned earlier, the PROM muscle would not respond with pain;
- Thoracic mobility is reduced – this can lead to overstressing the cervical area, as there is an interruption of joint functionality along the mobility and stability chain
- Whiplash accident – A whiplash is a fast stretch and contraction of the cervical ligaments, and it is a serious injury that needs to be addressed with specific mobility and strengthening exercises to prevent further pain and discomfort.
- Pain radiates from the neck to the shoulder – this is a common sign of cervical joint pain referral. The irritate area is painfully, but the pain signal does spread in the surrounding.
Conclusion for Joint Pain and Muscle Pain
To differentiate between Joint Pain and Muscle Pain, we have to use a series of observations that are based on objective and subjective findings, relative to the patient’s presentation.
While differentiating the source of the pain is a crucial step for the recovery and for stopping the pain, often, the final results is (from a prospective of a Clinical Myotherapist, but even a Physio or any other allied health) to give tools to the patients, in this case exercises, that can help the muscularscaletol structure to get stronger and more resiliant.
The case study provided above is a broad and simplified example of what we have to deal with on a daily basis as hands-on therapists. But of course, on top of the muscular scaletol pain and presentation, there are several other aspects that we have to consider when trying to manage pain, including lifestyle, stress level, sleep level and more. Some of those aspects are out of our scope of practice, and therefore, we can only suggest to the patient to seek extra care from their GP, which would then direct the patient to the right specialist.
Melbourne Massage and Treatment – Myotherapy Clinic
Lastly, if you are in pain and you are not sure what can help the most to get out of it, book a Myotherapy Initial consultation now, and let’s see what can be done about it.
At Melbourne Massage and Treatment, in Fitzroy North, during an initial consultation, we can track down the source of the pain and get to understand what can be done about it through hands-on treatment and exercise protocols. And if 1 to 3 sessions we can’t see any improvement, than would be worth it escalete this to a GP for further investigations, like a scan or a specialist referral.


Giovanni La Rocca
Giovanni moved to Melbourne, Australia, from Italy in 2008 and became a citizen in 2017. He started studying massage therapy in 2016, then completed a Bachelor of Health Science in Clinical Myotherapy in August 2024. During those years, he also specialised in Thai Massage and Manual Lymphatic Drainage for presentations like Lipoedema and Lymphoedema. Nowadays, he runs his clinic in Fitzroy North, Melbourne, where he integrates movement therapy into his practice to enhance overall well-being. He also values meditation, having completed several Vipassana courses. Committed to continuous learning, he aims to share his expertise in integrated therapies to help others achieve balance and resilience.