Patellar tracking disorder is a condition that occurs when the patella, also known as the kneecap, moves out of its original place when the leg straightens or bends.
What causes Patella Tracking Disorder?
In most cases, the kneecap shifts towards the outside of your leg, called “Lateral Patella tracking”.
Occasionally in some cases, it may shift toward the medial side too.
Why this shift happens due to the force applied to the kneecap itself.
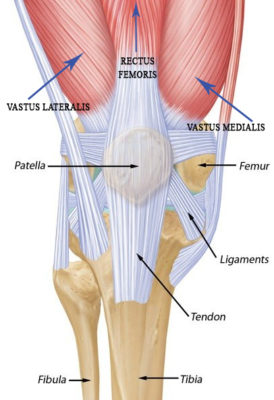
It was said that the knee joint is a hinge joint, which connects the tibia and fibula of your leg with the femur.
The kneecap is held in its natural position by ligaments on the medial and lateral sides and by tendons on the top side.
Below the patella is a cartilage layer that helps the patella glide along the femur’s groove.
When the cartilage below the patella does wear out, it can create pain and discomfort in the knee.
The misalignment of the patella results from tendons, muscles or ligaments that are either too tight or too loose.
Lateral patella tracking VS Medial patella Tracking
In the case of Lateral Patella Tracking, the Vastus Lateralist is over-developed compared to the Vastus Medialis or the IT Band (Iliotibial Band) pulling too much.
Vastus L. can overtake Vastus M’s strengthening due to the muscle size.
Indeed the V.L. is visibly bigger than the V. M.
On the other hand, tension along Gluteus Max and or tensions in the TFL can play a role in the pulling of the IT band.
Are you in Pain, and you suspect to have a Patella Tracking disorder? Get in touch with Giovanni now.
[contact-form][contact-field label=”Name” type=”name” required=”true” /][contact-field label=”Email” type=”email” required=”true” /][contact-field label=”Website” type=”url” /][contact-field label=”Message” type=”textarea” /][/contact-form]Risk factors for Patella Tracking Disorder
Here is a list of reasons that can lead to Patella Tracking Disorder:
- Footwear
- Running
- Weakness in the quads muscle
- Unbalance of muscle between the inner and outer regions of your tight
- Sports that require excessive knee bending, jumping or squatting
- Improper form or techniques while working out or during sports activities
- Overweight
- Genetics (structural reasons)
- Incidents or trauma to the knees
- Malformation within the femur bond
- Damaged cartilage
Symptoms
Pain is the most symptom of Patella tracking disorder.
The pain caused by this condition can occur during regular activity such as standing up, walking and or sitting down.
Any knee movement can recreate the pain.
In the case of arthritis, the pain can be more intense, and swelling is present at the knee joint.
Treatment Options
At Melbourne Massage and Treatment, the services available for Patella tracking are multiple.
Depending on the severity of the condition, Myotherapy treatment and or MLD are the most recommended.
Thanks to Dry Needling and/or Joint Mobilisation therapy, Myotherapy treatment can help rebalance the muscle forces surrounding the knee cap.
On the other hand, MLD can help in reducing the inflammation and the swelling present eventually on the knee joint.
What then Giovanni would look in, too, is also the mobility of ankles and hips.
The correct mobility of these two joints would ensure that the knee is not compensating for the poor joint quality of movement, which can be part of why the patella tracking disorder is in the first place.


Giovanni La Rocca
Giovanni moved to Melbourne, Australia, from Italy in 2008 and became a citizen in 2017. He started studying massage therapy in 2016, then completed a Bachelor of Health Science in Clinical Myotherapy in August 2024. During those years, he also specialised in Thai Massage and Manual Lymphatic Drainage for presentations like Lipoedema and Lymphoedema. Nowadays, he runs his clinic in Fitzroy North, Melbourne, where he integrates movement therapy into his practice to enhance overall well-being. He also values meditation, having completed several Vipassana courses. Committed to continuous learning, he aims to share his expertise in integrated therapies to help others achieve balance and resilience.