In Victoria, Lymphoedema patients are entitled to access the SWEP program (State Wide Equipment Program), a government-funded program that provides funding for garment wear on an annual basis. As a Myotherapist and Lymphoedema therapist working in Fitzroy North, I can help you overcome the bureaucracy and understand how to access the SWEP incentives and where to go and purchase the garments. What Is the SWEP Program? The SWEP or State-Wide Equipment Program is a Victorian government-funded scheme that provides subsidised or fully funded medical equipment to eligible individuals living with permanent or long-term conditions, and Lymphoedema is one of these conditions. For those who live with a chronic condition like lymphoedema, the SWEP can significantly reduce the financial burden of compression garments, which are an essential, not optional, part of lymphoedema management. So yes, SWEP is not a treatment program but an equipment funding pathway. Why Compression Garments Are Essential for Lymphoedema Lymphoedema is a lifelong condition, and unfortunately, in most cases, it is not curable. For managing this presentation, therapies like Manual Lymphatic Drainage (MLD) and Complete Decongestive Therapy (CDT) can help reduce the swelling, and then compression is what maintains results. Without appropriate compression: Swelling returns Tissue becomes heavier and more fibrotic Skin integrity is compromised Infection risk (cellulitis) increases This is why access to properly fitted garments through programs like SWEP is so important. What Lymphoedema Items Can Be Funded Through SWEP? The SWEP may assist with funding for: Compression garments (flat knit or circular knit, based on clinical need) Wrap systems Custom-made garments when off-the-shelf options are unsuitable The funding is based on: Medical necessity Functional impact Long-term condition status Financial eligibility The SWEP does not automatically cover all the costs, as approval depends on correct documentation and assessment, and that’s where I can assist you. Below you will find a section dedicated to the cost covered by SWEP via the Lymphoedema Compression Gargments Program (LCGP). SWEP and Lymphoedema Compression Garment Program (LCGP) In Victoria, patients with lymphoedema can access the Lymphoedema Compression Garment Program (LCGP) via SWEP. Indeed, SWEP and LCGP are 2 separate programs, but it is SWEP that took control of the LCGP in 2017, and this is how it works. LCGP is funded by the Department of Health and provides subsidised compression garments and wrap systems for eligible individuals diagnosed with primary, secondary, or sub-clinical lymphoedema affecting the limbs. What Is Funded Under the LCGP? From the day of submission to the SWEP for the garment wear, you have 12 months to get funding for: Adults 4 sets of compression garments per affected limb, or 3 sets of compression garments and 1 kit of Adjustable Wrap Systems (AWS) per affected limb, or 2 kits of Adjustable Wrap Systems (AWS) per affected limb 1 donner (once off) Children under 18 years of age 6 sets of compression garments per affected limb, or 5 sets of compression garments and 1 kit of Adjustable Wrap Systems (AWS) per affected limb, or 2 kits of Adjustable Wrap Systems (AWS) per affected limb 1 donner (once off) Available Subsidies Those above are the number of garments you get funding for, and each garment is subsidised as follows: Ready to Wear (RTW):$150 per set of garments per affected limb Made to Measure (M2M):$300 per set of garments per affected limb where RTW is not compatible with limb size, shape, or required compression class Adjustable Wrap Systems (AWS) kit:$150 per kit Donner (once off):$60 Who Is Eligible for State Wide Equipment Program? To be eligible for SWEP in Victoria, you must: Are a permanent Victorian resident, hold a temporary or permanent protection visa, or are an asylum seeker Have a long-term condition or disability, and/or are frail aged Do not receive other government funding for compression garments Are not an inpatient of a public or private hospital, or a permanent resident of a residential care facility Cannot claim garments through private health insurance Have not been discharged from a public hospital or extended care centre within the last 30 days, where garments relate to the hospital admission Further assistance with determining your eligibility can be obtained via this link, which directs you to the SWEP website’s Check Eligibility page. My Role in Supporting SWEP Applications At my Lymphoedema clinic in Fitzroy North, I regularly support patients by: Performing comprehensive lymphoedema assessments Identifying the correct compression type and class Providing clinical justification for garments Working alongside GPs and specialists for referrals (my clinic is situated in a GP clinic) Ensuring garments align with the patient’s stage of lymphoedema and lifestyle needs As a lymphedema practitioner, I trained with the Vodder Academy for Lymphoedema Management, so I do understand the importance of precise garment selection, not just eligibility. On the other hand, I am also a member of the Australasian Lymphology Association (ALA), and I stay aligned with current best-practice standards when recommending compression solutions. SWEP Is Not a Substitute for Treatment Another important point that I want to mark again is that SWEP does not replace therapy. What this means is that for the best outcomes, compression garments should be used alongside: Manual Lymphatic Drainage (MLD) Complete Decongestive Therapy (CDT) Skin care Movement and load management Ongoing review and garment reassessment In fact, compression works best after swelling has been optimally reduced, not as a standalone solution. This is because compression, applied to a non-managed Lymphoedema, may result in hard to apply, can crack the skin (which would lead to infections), and it may also be painful. SWEP in Fitzroy North At Melbourne Massage and Treatment, Myotherapy & Lymphoedema clinic in Fitzroy North, I support patients with evidence-based care, practical guidance, and individualised planning, so you can manage lymphoedema with confidence. If you’d like support with SWEP-related compression, assessment, or ongoing lymphoedema management, use the button below to book a FREE 15-minute online consultation (Option 9).
Tag Archives: Lymphoedema
Compression therapy is essential for lymphoedema management, and therefore, is worth it write a blog where we are going to talk about what compression is ideal for what lymphoedema presentations, including the mmHg levels. I’m Giovanni, and I run Melbourne Massage and Treatment, a Myotherapy and Lymphoedema clinic in Fitzroy North. I trained with the Vodder Academy in lymphoedema management, and I provide Complete Decongestive Therapy (CDT), which forms the foundation of effective lymphoedema treatment. What Does mmHg Mean in Lymphoedema Compression? As when measuring blood pressure, even when working with Lymphoedema, we use the measuring unit mmHg (millimetres of mercury) when talking about compression. Based on the type of presentation, as lymphoedema therapists, we would recommend different types of compression garments, including flat knit or circular knit. So, here is a short list of the purposes of compression garments: Support the lymphatic system Encourage lymphatic flow Prevent fluid from re-accumulating Maintain the results achieved through CDT Therefore, choosing the correct mmHg compression level is about balancing effectiveness, safety, and comfort, and not only apply some form of pressure on the affected limb. Compression Classes and Lymphoedema Management To simplify how compression garments work, companies like Sigvaris or Juzo grouped the compression into classes or levels, each corresponding to a specific mmHg range. Common Compression Levels Used in Lymphoedema Compression Lower compression levels – 15–20 mmHgOften considered in: Mild lymphoedema Early-stage swelling Fragile or sensitive skin Situations where tolerance is limited Moderate compression levels – 20–30 mmHgCommonly used for: Established lymphoedema Post-intensive CDT Long-term volume maintenance Daily functional support Higher compression levels – 30–40 mmHgUsually required for: Moderate to severe lymphoedema Fibrotic or hardened tissue Significant limb shape changes Swelling that rebounds quickly My personal suggestion is that the correct Compression Level should always be determined following a thorough clinical assessment, in order to avoid fluid retention and waste of money. Why Higher Compression Is Not Always Better Compression level in lymphoedema treatment, as mentioned above, has to be a balance of effectiveness and comfort, and different presentation, with or without fibrosis, mobile or immobile limb, comes with different compression needs. Indeed, applying the wrong type of compression can: Reduce comfort and compliance Increase skin irritation or skin breakdown Compromised lymph circulation Make garments difficult to don and doff In fact, effective Lymphoedema Compression works with the body, not against it, and that’s why for lymphedema presentation compression garments are recommended to be worn after taking specific measurements, that ensure a gradient pressure is applied on the limb, so that the lymph fluid is pushed in the right direction and not towards the extremity of the limb. Compression Levels and Complete Decongestive Therapy (CDT) At Melbourne Massage and Treatment, as part of lymphedema management, I offer MLD as a manual therapy to stimulate the lymphatic system, and CDT (Complete Decongestive Therapy), to reduce the swelling and limb size. More specifically, CDT, can help with: Reduce swelling after the delivery of Manual Lymphatic Drainage (MLD) Improve tissue quality Shape the limb appropriately Prepare the limb for long-term Lymphoedema Compression Help in the breakdown of fibrosis Once the limb has stabilised, compression garments help maintain volume reduction and prevent progression of lymphedema. Professional Assessment Is Essential Certain pharmacies or retail shops (including online one) may sell compression garments, but those are probably not specific enough for a Lymphoedema presentation. Indeed, the appropriate Compression Level depends on: Lymphoedema stage Limb shape and size Tissue texture and fibrosis Skin condition Functional needs and daily activity For compression garments, post MLD and CDT therapies, I refer patients to Sigvaris in West Melbourne, which specialises in medical compression for lymphoedema and ensures accurate fitting and garment selection. Lymphoedema Compression in Fitzroy North Living with lymphoedema can be challenging, and you may find yourself in need of ongoing care and help in navigating information regarding the right compression strategy. At Melbourne Massage and Treatment in Fitzroy North, I provide: Evidence-based CDT Personalised lymphoedema management Clear guidance on Lymphoedema Compressions Collaborative care with trusted compression garment providers So if you’re seeking professional lymphoedema treatment in Melbourne, or want clarity around compression levels and mmHg, I’m here to help. Accessing Compression Garments Through the SWEP Program For some people living with lymphoedema, the cost of Lymphoedema Compression garments can be a barrier to effective long-term management. In Victoria, eligible patients may access support through the State-Wide Equipment Program (SWEP), which provides funding for medically necessary aids, including compression garments for lymphoedema. As a Clinical Myotherapist, I can help you go through the SWEP program in collaboration with your GP. The role of the GP is to write a diagnosis and a referral to the SWEP program, and that’s where I can assist them. After that, you can refer to an approved compression provider, such as Sigvaris in West Melbourne, who can advise on garment selection and fitting. The Swep program for Lymphoedema patients can help with: Reduces the cost of Lymphoedema Compression garments for eligible patients Supports long-term lymphoedema management after Complete Decongestive Therapy (CDT) Ensures clinically appropriate compression through professional assessment FAQ – Lymphoedema Compression Levels
Once you have been diagnosed with lymphoedema (also known as lymphedema), you will soon learn that compression therapy plays a vital role in long-term management of this chronic condition, and one of the most common questions I hear in my clinic is: “What’s the difference between circular knit and flat knit lymphoedema compression garments?” In this blog, I will explain the difference between these two types of lymphoedema compression knit, so that it may help you understand better how your lymphoedema can be managed in the long term. Why Is Lymphoedema Compression Essential? As discussed in many more blogs, lymphoedema is a chronic condition caused by an impaired lymphatic system, which leads to the accumulation of lymph fluid and persistent swelling in one or more body parts. If not correctly managed, lymphoedema can progress and cause: Increased limb size – elephant leg Tissue fibrosis (hardening) Skin changes – including numbness Higher risk of infections – cellulitis is a common one Compression therapy is a cornerstone of CDT (Complete Decongestive Therapy), alongside: Manual Lymphatic Drainage (MLD) – ideal to boost your lymphatic system drainage capacity Skin care is essential to avoid skin cracks and infections Exercise and movement – especially if wearing circular knit compression Long-term compression – So in short, lymphedema compression supports lymphatic flow, helps maintain limb volume reduction, and prevents the worsening of lymphoedema. What Is Circular Knit Lymphoedema Compression? Circular knit compression refers to the method by which garments or bandages are made. In this case, the knit is made using a continuous circular weaving method, creating a seamless and highly elastic fabric. Benefits of circular knit compression: Lightweight and smooth texture Greater elasticity and stretch Often available off-the-shelf More discreet under clothing Circular knits are ideal for those lymphoedema patients who can and should move with the limb affected by lymphoedema. Indeed, the circular knits are designed to allow the lymphedema patient to move; therefore, while the limb is compressed, the lymphatic system is simultaneously boosted by compression and movement. When circular knitting may be suitable: Mild lymphoedema Early-stage lymphedema Limbs with minimal shape distortion Well-controlled swelling However, due to their elasticity, circular knit garments often lack the containment needed for more advanced lymphoedema, especially when fibrosis or limb shape changes are present. What Is Flat Knit Lymphoedema Compression? So, even in the case of Flat-knit compression, the name refers to the way the fabric is produced, like flat fabric and stitched together with a seam. This allows for higher stiffness and customised shaping. Benefits of flat knit compression: Firmer, more supportive structure Superior containment of swelling Custom-made to individual limb measurements Better control of irregular limb shapes Flat knit is usually recommended for: Moderate to severe lymphoedema Long-standing or progressive lymphedema Skin folds or lobes Fibrotic tissue Swelling that rebounds quickly A lymphoedema patient is unable to move much Therefore, based on the severity and lymphoedema stage, we would suggest using flat knit compression for more severe presentations or for someone who is unable to move the limb(s) affected. Compression Garments and Complete Decongestive Therapy (CDT) At Melbourne Massage and Treatment, in Fitzroy North, I offer Complete Decongestive Therapy (CDT) as part of lymphoedema management, which is internationally recognised as the most effective approach to lymphoedema treatment. Here is a list of things that I would offer during a lymphoedema management appointment: Comprehensive lymphedema assessment Manual Lymphatic Drainage Swelling reduction during the intensive phase of CDT Preparing limbs for compression garments Education on long-term self-management To simplify the process of lymphoedema management, at Melbourne Massage and Treatment, I do offer a free 15-minute online consultation, where I can answer your questions and go through an initial assessment about your clinical history. Compression After CDT After we manage to reduce the swelling in the limb(s) affected by lymphoedema, via MLD and CDT, which can take 3 to 5 appointments, or more, depending on your presentation, we can then look into getting garment wear that can fit your limb(s), so that the swelling can be managed for a longer time. While I do not supply compression garments directly, I refer patients to Sigvaris in West Melbourne, specialists in medical compression for lymphoedema, ensuring accurate fitting and high-quality garments. Circular Knit vs Flat Knit: Which Is Right for You? The correct compression garment depends on several factors, including: Stage and severity of lymphoedema Limb shape and tissue texture Presence of fibrosis Skin health Lifestyle and daily activity This is why coming for an appointment and getting your lymphoedema assessed and treated, where needed, is essential before selecting compression. Lymphoedema Treatment in Fitzroy North Living with lymphoedema can be challenging, but with the proper care, education, and treatment plan, it can be effectively managed. At Melbourne Massage and Treatment in Fitzroy North, I focus on: Evidence-based CDT Individualised lymphedema management Clear guidance around compression therapy Collaborative care with trusted garment providers Therefore, if you are in need of professional lymphoedema treatment in Melbourne or need clarity around compression options, I’m here to support you. About myself: a Myotherapist specialised in Lymphoedema Management My name is Giovanni, and I run Melbourne Massage and Treatment, a Myotherapy and Lymphoedema clinic in Fitzroy North. I trained with the Vodder Academy in lymphoedema management, and I provide Complete Decongestive Therapy (CDT), the gold standard for lymphedema treatment. My approach is tailored to each individual patient, to achieve objective results, and to help you enjoy more your life while dealing with Lymphoedema management.
As a Myotherapist and Lymphoedema Therapist here in Fitzroy North, I’ve always believed that movement is one of the most powerful tools for health. Exercise isn’t just about getting fit; it’s about feeling stronger, moving with ease, and living life without pain. Recently, I completed professional training in Kinetic Link Training (KLT), and it gave me the opportunity to see fitness classes and rehabilitation programs under a new light. I’m now offering KLT sessions in Fitzroy North as part of my fitness class at Melbourne Massage and Treatment, in order to help clients move better, recover well, and build long-term strength. Why Exercise Is Good for Everyone The benefits of regular exercise are many, including: Improves muscle tone; Boosts energy Supports joint health; Improves posture; Reduces stress So it doesn’t matter what your goal is, whether you are recovering from an injury, working a desk job, or simply wanting to feel stronger, functional movement training is one of the best investments you can make in your health. That’s why we said that movement is medicine. And Kinetic Link Training is ideal for any fitness level, given the simplified structure of its exercises, and the fact that its setup can be easily replicated at home with some resistance bands and some light dumbbells. How Kinetic Link Training Is Different from Conventional Training More traditional gym workouts often aim to work one group of muscles at a time, with a primary focus on agonist muscles, agonist to a certain movement, such as bicep curls, leg presses, and shoulder raises. Nothing wrong with those exercises, they definitely help you build strength, yes, but not always functional strength. That’s where Kinetic Link Training is different, as KLT is built around integrated, full-body movement patterns that connect the upper and lower body through controlled, coordinated actions. Instead of training one movement at a time, you train the body as a connected system. This style of training improves: Core stability and posture Joint mobility and balance Real-world strength and coordination To simplify it, KLT helps you move better, not just lift more. Therefore, having a goal in mind when choosing to start training can help you define the type of training you may need and want to go for. Kinetic Link Training Is Also Ideal for Post-Surgery and Injury Recovery Rehab KLT is an excellent option for rehabilitation and post-surgery recovery. A few keys component that makes KLT so safe are: Low-impact exercises Controlled movement Entirely adjustable for your needs You can train easily at home What then makes KLT effective for rehabilitation is the fact that you will be asked to do natural movement patterns that can help in regaining body strength safely. In fact, KTL is ideal for anyone looking to rebuild function, improve range of motion, and return to daily activity with confidence. Perfect for Beginners and Those New to Strength Training If you’ve never done strength training before, KLT is a gentle and intelligent place to start. “Why so?” you may ask. Well, the beauty of KLT is that it allows you to perform any exercise to your capacity, and from there, you can not only increase the load or resistance, but you can also increase the degree of movement. Let’s take, for example, a posterior pull with a double leg squat: In this exercise, you are going to start in a squat position (max depth is quads parallel to the ground), facing the machine or the cable direction, while your arms are fully extended. To deliver the exercises, you will be asked to stand while pulling the cable towards yourself, with the elbows running alongside the ribcage. Now, let’s consider a person who may have difficulty squatting. They are not required to go as deep to start with, but still, they can apply a full upper body range of motion, which is basically like a lat. raw exercise. The depth of the squat would come with time and practice. This is only an example of how exercises can be adapted You don’t need to be strong, flexible, or experienced. The movements are easy to learn and can be scaled to any fitness level. Kinetic Link Training: A Balanced Full-Body Workout Now, another great advantage of KLT is the engagement of the upper and lower body in all its exercises. As explained in the example above, along with the KLT exercises, you are required to engage in: Upper body movement: Push Pull Arch Double or Single arm. Different directions, “from where” and “to where” the cable may run: Very Low Low Mid High Very High With or without crossover. Lower body movement between: Squat – Double Leg, Single Leg, Wide Stand Lunge – Anterior, Posterior, Lateral Calf Raises (as a progression of the end/start of squat movement) Which can also be subcategorised as alternated, Split, Reciprocal, and Partial Standing direction: 0° – Facing the cable 45° – To the cable 60° – To the cable 90° – Your L/R side is facing the cable direction 180° – You are giving your back to the cable direction Now, combine all of those options, and you easily end up with thousands of exercises that engage the upper and lower body with an incredible variety of regression and progression. Indeed, this is why every KLT session integrates upper and lower body movements, creating balanced, total-body strength. This ensures you don’t overwork one area while neglecting another. KLT and Lymphoedema Lymphoedema is a chronic condition characterised by severe swelling of the limb due to failure of the Lymphatic System. It can occur due to a congenital presentation (primary Lymphoedema) or post-surgery (secondary Lymphoedema), as often happens after cancer surgery. To manage a Lymphoedema presentation, exercises are essential, as the lymphatic system is stimulated by muscle contraction. Based on the severity of your lymphedema, we can use KLT to help you boost lymphatic fluid circulation and build resistance in the joints and limbs affected by lymphedema. Functional Fitness Fitzroy North Bringing Kinetic Link Training into my practice […]
As a Lymphoedema therapist, I often get asked what the difference is between Lymphoedema and Lipedema. In this blog, we will explore the differences, the similarities, and what can be done for prevention, management and treatment of those presentations. Furthermore, we will look into how Lipoedema can degenerate into a Lipo-Lymphoedema, and why this is not the case for everyone. What is Lipoedema? Lipoedema is a chronic adipose tissue disorder that primarily affects women. On a global scale, we know that about 11% of women are affected by this presentation, and it often runs in families as it has a strong genetic component. The major characteristics of Lipoedema are an abnormal and symmetrical accumulation of fat around the hips, buttocks, thighs, and legs, and upper arms. On the leg area, the fat appears in abundance in the medial side of the knee, too. Where feet are completely untouched by the fat accumulation, this fat is resistant to diet and exercise and is often painful to touch. The pain is due to the cutaneous nerve entrapped in the fatty tissue, and so delivers a pain response when stimulated. Other Lipoedema key features: Often triggered or worsened by hormonal changes Symmetrical fat distribution Soft, nodular, or lumpy tissue Pain and easy bruising – as per the pain, bruising is due to blood capillary compression from the fat, and so, is easily damaged by touch No skin thickening or pitting in the early stages Nowadays, there is increasing awareness about this presentation, and more and more women find benefit from a management protocol that is not only about cardio and exercise. Part of the Lipoedema management includes: Movement Compression stocking Antiinflammatory diet Skin care Where and if needed, cosmetic surgery intervantion What is Lymphoedema? Lymphoedema, on the other hand, is a condition where lymphatic fluid builds up in the tissues due to a malfunctioning lymphatic system, causing chronic swelling. Compared to Lipoedema, Lymphoedema is strictly related to the Lymphatic system. It can be primary (congenital or hereditary) or secondary (due to trauma, surgery, radiation, or infection affecting the lymphatic system). Lymphoedema characteristics: Unilateral or asymmetrical swelling (though it can be bilateral) Pitting edema – It consists of deep indentation (pitting) left behind on the skin when pressure is applied Skin changes over time (fibrosis, hyperkeratosis, papillomatosis) Affects feet and hands as well – primary lymphedema would start from the extremity Heaviness or tightness in the affected area – can potentially be pain-free, but the limb/s may feel very heavy It does affect men and women – only primary lymphedema has a genetic component Lymphoedema Management The management of Lymphoedema is more tricky than lipoedema, as everyone may react differently to the management, it can be related to other health issue which needs to be considered, and requires the patient to be active in the management side of things. At Melbourne Massage and Treatment, I treat different types of lymphedema, as per the upper and lower body, focusing on an initial reduction of the swelling via a combination of Manual Lymphatic Drainage (MLD) and compression with Combined Decongestive Therapy (CDT). The management of this presentation can take anywhere between 3 and 5 or more appointments, depending on the severity of the presentation. The treatments are better done in close proximity, 24 to 48 hours one after the other, so that we give no time to the body to accumulate fluid back under the skin. Once the combination of treatment allows us to achieve the desired result, which is bringing the limb/s to a thinner size, you will be scheduled for a custom garment wear compression, which will guarantee to maintain the results achieved. This is usually done at other clinics, like Sigvaris or Juzo clinics. Those clinics are specialised in the making of garment wear. Custom garments wear last about 6 months, so twice a year, you will need to change them, and if needed, because the limb/s may start swelling again (especially in summer, when there is a change of atmospheric pressure, due to the heat), a short series of MLD and CDT therapy may be needed. Key Differences between Lymphoedema and Lipoedema Feature Lipedema Lymphoedema Cause Abnormal fat metabolism Lymphatic dysfunction Gender prevalence Almost exclusively women Affects both sexes Onset Often at puberty, pregnancy, or menopause Can be congenital or triggered by injury/surgery Distribution Symmetrical, lower limbs and arms Can be asymmetrical; any body part Feet/Hands Spared Usually involved Pain Tender, painful fat Often painless, heavy feeling Skin texture Soft, nodular fat Skin thickens over time (fibrosis) Pitting Rare (early) Common (early) Response to elevation Minimal improvement Often improves with elevation (if early stage) Bruising Common Not typical Common Characteristics of Lymphoedema and Lipoedema As seen above, the characteristics of Lipoedema and Lymphoedema are different, but, both conditions share chronic swelling, potential functional limitations, and a need for long-term management: Both can cause leg discomfort, heaviness, and swelling Both may lead to reduced mobility Neither condition improves with calorie restriction or exercise alone – it is more about stop the intake of inflammatory food Compression therapy is often used for both Both can have a progressive nature if not managed properly – especially lymphoedema Misdiagnosis is common, often delaying effective treatment When Lipedema Becomes Lipo-Lymphoedema If we stick to a vision of Lipoedema progression, that is possible when no management is put in place, this presentation can degenerate into secondary lymphatic impairment, resulting in a combined condition known as Lipo-Lymphoedema. How this happens: As the fat keeps accumulating under the skin, and there is an increase in inflammation, the lymphatic vessels are put under major load and potential damage Over time, this leads to fluid retention and swelling due to the lymphatic system failing to do its job As the lymphatic system becomes overwhelmed, the person may start experiencing lymphedema symptoms (Example: swelling in the extremities, feet and or hands) Patients now experience both fat deposition and fluid buildup, making treatment more complex Signs that Lipedema has progressed: Swelling starts in the feet […]
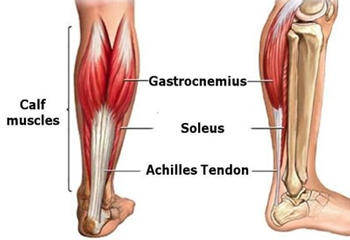
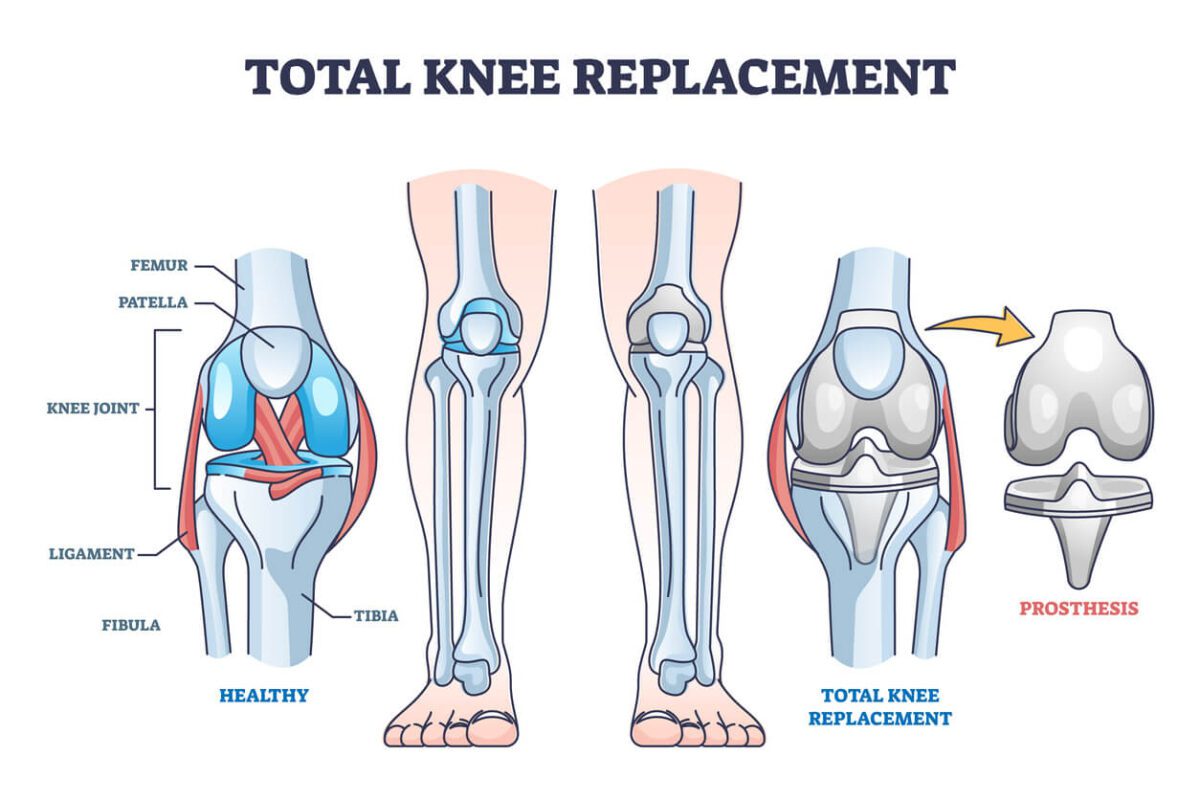
Knee replacement surgery, or knee arthroplasty, is a transformative procedure designed to alleviate pain and restore function in patients suffering from severe knee damage. While the surgery is a crucial step toward improved mobility, the journey doesn’t end in the operating room. The rehabilitation process is vital for ensuring a successful recovery and regaining your pre-surgery quality of life. A key component of this recovery is Manual Lymphatic Drainage (MLD) and a tailored exercise program. Understanding Knee Replacement Surgery Knee replacement surgery as the name says, is basically the replacement of a damaged knee joint with an artificial one. There are two type of knee replacement surgery: a total knee replacement (TKR), which replaces the entire knee joint, or a partial knee replacement, which targets only the damaged part of the joint. Nowadays, the decision to undergo knee replacement surgery is often made when conservative treatments, such as medications and physical therapy, have failed to provide relief. This is because, we are more aware now than ever, of how surgery are complex intervention that can yes, give pain relief and benefit, and save life, but occasionally can come with complications and leave the person with other permanent damage. The Rehabilitation Process As in any surgery, the rehabilitation process is extremely important to ensure that the patient returns to the best of their functions. What the rehabilitation involves are physical therapy, exercises, and, where needed, even mental support. Immediate Post-Surgery Care: Pain Management: Right after your surgery, you will be given pain relief medications and antibiotics, which will help in managing the pain response and keep you free from infection risks. Initial Movement: As a few days are pass, is super important to start moving. Initially would be a matter of few mm or cm, passive and active movement, but as days goes by these movement has to be increased, in order to avoid further muscle atrophization and to increase the blood flow to the area. Exercise: Isometric Exercises: As per discussed in many other blogs, those exercises are the first step in the recovery process. An isometric exercise consists of muscle contraction and barely any limb movement. This allows for maintaining a connection between the muscle and the Central Nervous System (CNS), which is essential to ensure muscle engagement for more complex tasks. Initially, those exercises can be achieved with only 25% of your strength, and within 10 days post-surgery, you may start pushing at 50% of your strength or more. Strengthening Exercises: This second step in the exercise journey can start in week three or four after surgery. The process focuses on strengthening the muscles surrounding the knee joint. These exercises are essential for supporting the new joint and improving overall stability. Strengthening exercises may look different from person to person, in terms of load, but they all aim to increase the load to which the knee joint is placed, to stimulate muscle growth, blood flow, and restore all tissue damaged along the surgery. Plyometric Exercises: Lastly, along the rehabilitation process, there are the plyometric exercises, which consist of loading the tendon like a spring (that’s what their function is) and releasing that loading in a fast motion. For a knee joint, think of explosive squat-type exercises. These type of exercises would start around week 8 to 10 post surgery. This is a step-by-step guide of what a rehabilitation process may look like. Each individual then may have a different journey to follow, given their clinical history, and other factors, including genetics and return to daily activities. In addition to the exercises, physical therapy Consistency: Adhering to a home exercise program is crucial for maintaining progress during therapy sessions. Monitoring Progress: Regularly perform your home exercises and track your progress. If you encounter any issues or experience increased pain,get in touch with your physical therapist to discuss what you are presenting with and what can be done about it. Monitoring and Follow-Up: Your surgeon and physical therapist will evaluate you on an ongoing basis to ensure that your recovery is progressing as expected. Any complications or concerns will be addressed promptly. The Importance of Manual Lymphatic Drainage (MLD) Manual Lymphatic Drainage (MLD) is a gentle, hands-on therapy designed to stimulate the lymphatic system and reduce swelling, which can be particularly beneficial following knee replacement surgery. Here’s how MLD supports recovery: Benefits of MLD in Knee Replacement Recovery: Reducing Swelling: Fluid Management: Swelling or edema is a common issue after knee replacement surgery. MLD helps move excess fluid away from the surgical site and reduces overall swelling, which can enhance comfort and mobility. Enhancing Circulation: Improved Blood Flow: By promoting lymphatic flow, MLD also improves blood circulation, delivering essential nutrients and oxygen to the healing tissues, which supports a faster recovery. Reducing Pain and Discomfort: Pain Relief: The gentle massage techniques used in MLD can help alleviate pain and discomfort associated with swelling and inflammation, contributing to a more comfortable recovery experience. Facilitating Faster Recovery Helping the Healing: By reducing swelling and improving circulation, MLD can lead to a more efficient recovery process, enabling more effective physical therapy and exercise. Incorporating MLD into Your Rehab Routine Timing: MLD can be introduced a few days to a week after surgery, depending on your surgeon’s recommendations and your individual healing progress. How can I help? At Melbourne Massage and Treatment, as a Clinical Myotherapist I am trained in helping people recovering from knee surgery or other major surgeries, either with Fitness Class, which can be part of a Myotherapy treatment plan, but even via treatment like Manual Lymphatic Drainage. So if you are about to get a surgery, that is a knee replacement or any other surgery, and you are looking for someone that can assist you with your recovery, get in touch now to discussed your needs and I can give you a rund down on how I will be able to help you. Knee replacement surgery and lymphoedema. As mentioned earlier, we can all have different outcomes from the […]
Lymphoedema and Lipoedema are chronic conditions characterised by swelling and fat accumulation, respectively, often accompanied by inflammation. Thanks to emerging research, we do not know that dietary choices, particularly the consumption of long-chain fatty acids, can influence the inflammatory processes associated with these conditions. This is why it is important to consider an Anti-Inflammatory Diet when suffering from those presentations. The Role of Long-Chain Fatty Acids in Inflammation Long-chain fatty acids are absorbed into the lymphatic system in structures called chylomicrons. Once these chylomicrons are processed, the released fatty acids can interact with macrophages—immune cells responsible for detecting and responding to pathogens. This interaction can trigger an inflammatory response, contributing to the chronic inflammation observed in both lymphoedema and Lipoedema. Why does the Lymphatic System absorb Long-Chain Fatty Acids? The lymphatic system plays a crucial role in the absorption and transport of dietary fats, particularly long-chain fatty acids. This process is essential for efficient lipid metabolism and overall energy distribution in the body. Absorption of Long-Chain Fatty Acids Long-chain fatty acids are released from dietary fats in the small intestine during digestion. These fatty acids are absorbed by the enterocytes (intestinal cells), where they are reassembled into triglycerides and packaged into lipoprotein particles known as chylomicrons. Due to their size and composition, chylomicrons are too large to enter the blood capillaries directly. Instead, they are absorbed into specialized lymphatic vessels called lacteals, located within the villi of the small intestine. This lymphatic absorption allows the efficient transport of large lipid molecules into the systemic circulation. Transport Through the Lymphatic System Once inside the lacteals, chylomicrons travel through the lymphatic system, merging into larger lymphatic vessels and eventually entering the bloodstream via the thoracic duct, which empties into the left subclavian vein near the heart. This pathway enables the gradual release of lipids into the circulation, allowing tissues to access these essential nutrients for energy production, cell membrane synthesis, and other vital functions. Benefits of an Anti-Inflammatory Diet Adopting an anti-inflammatory diet can help mitigate these effects by reducing the intake of pro-inflammatory long-chain fatty acids and emphasising foods that support lymphatic health. Key components of such a diet include: High Fibre Intake: Consuming fruits and vegetables rich in fibre promotes the production of short-chain fatty acids in the gut, which have anti-inflammatory properties. Omega-3 Fatty Acids: Incorporating sources of omega-3s, such as fatty fish, flaxseeds, and walnuts, can reduce inflammation and edema. Anti-Inflammatory Spices: Spices like turmeric, garlic, and curry leaves possess natural anti-inflammatory effects and can be beneficial additions to the diet. Foods to Limit or Avoid for a Good Anti-Inflammatory Diet To further reduce inflammation, it’s advisable to limit the consumption of: Processed Foods: Often high in trans fats and refined sugars, these can exacerbate inflammatory responses. Excessive Salt and Caffeine: High intake of salt and caffeine may contribute to fluid retention and should be moderated. Alcohol and Sweets: These can increase inflammation and are best consumed in moderation. Personalised Nutritional Guidance As a certified lymphoedema therapist trained by the Vodder Academy, I understand the importance of a holistic approach to managing lymphoedema and Lipoedema. Integrating an anti-inflammatory diet tailored to your individual needs can play a crucial role in reducing inflammation and improving overall health. For personalised advice and support, consider consulting with a healthcare professional or a registered dietitian experienced in managing these conditions. By making informed dietary choices, you can actively contribute to managing inflammation and supporting your lymphatic health. For more insights on managing lymphoedema and Lipoedema through diet, you might find this video informative. Melbourne Massage and Treatment and Lymphoedema/Lipoedema presentation Even though I am not a dietitian or nutritionist, so I can not give any direct recommendations on your diet or food intake, as a Lymphoedema therapist, I can still help you manage your presentation by offering services like Manual Lymphatic Drainage (MLD) and Combined Decongestive Therapy (CDT). So, if you need to improve your Lymphoedema or Lipoedema presentation, book your free 15-minute phone consultation now to understand how Melbourne Massage and Treatment services can benefit you. FAQ about Anti-Inflammatory Diet and Lymphoedema/Lipoedema presentation Q: How do dietary choices influence inflammation in lymphoedema and Lipoedema? A: Dietary choices play a significant role in modulating inflammation associated with lymphoedema and Lipoedema. Consuming foods high in long-chain fatty acids can lead to their absorption into the lymphatic system, where they may interact with macrophages—immune cells responsible for detecting and responding to pathogens. This interaction can trigger an inflammatory response, contributing to the chronic inflammation observed in both conditions. Adopting an anti-inflammatory diet can help mitigate these effects by reducing the intake of pro-inflammatory foods and emphasizing those that support lymphatic health. Q: What are long-chain fatty acids, and how do they affect inflammation? A: Long-chain fatty acids are a type of fat molecule commonly found in various foods, including certain oils, meats, and processed products. When consumed, these fatty acids are absorbed into the lymphatic system in structures called chylomicrons. Once processed, the released fatty acids can interact with macrophages, triggering an inflammatory response. This process can exacerbate the chronic inflammation associated with lymphoedema and Lipoedema. Q: Which foods are high in long-chain fatty acids and should be limited? A: Foods rich in long-chain fatty acids that may promote inflammation include: Certain oils Meats Processed products Limiting the intake of these foods can help reduce inflammation. Q: What are the key components of an anti-inflammatory diet that are beneficial for lymphoedema and Lipoedema? A: An anti-inflammatory diet focuses on incorporating foods that help reduce inflammation and support lymphatic health. Key components include: High Fibre Intake: Consuming fruits and vegetables rich in fibre promotes the production of short-chain fatty acids in the gut, which have anti-inflammatory properties. Omega-3 Fatty Acids: Incorporating sources of omega-3s, such as fatty fish, flaxseeds, and walnuts, can reduce inflammation and edema. Anti-Inflammatory Spices: Spices like turmeric, garlic, and curry leaves possess natural anti-inflammatory effects and can be beneficial additions to the diet. Q: Are there specific foods I should […]
Hello, and welcome! I’m Giovanni, and today I want to share some insight into the available treatment options for lymphoedema. If you or someone you know is dealing with this condition, I understand how overwhelming it can feel to navigate the many different approaches to treatment. As someone specialising in lymphoedema management through Manual Lymphatic Drainage (MLD) and Complex Decongestive Therapy (CDT), I aim to provide a holistic approach to managing and reducing the symptoms of lymphoedema. I’ve studied with the Vodder Academy and am a Clinical Myotherapist, so my work is built on solid, evidence-based practices. But I also believe that looking at all available treatment options for lymphoedema —medical, surgical, and holistic—is key to finding a management strategy that works for you. What is Lymphoedema? Before we dive into treatment options, let me quickly touch on what lymphoedema is. Lymphoedema is a condition that causes fluid retention and swelling, usually in the arms or legs, as a result of damage or blockage to the lymphatic system. This can occur after surgery, radiation treatment, or due to inherited conditions. While lymphoedema may be chronic, the good news is that with the proper treatment, symptoms can often be managed or reduced significantly. Medical Treatment Options for Lymphoedema Medical treatments for lymphoedema typically focus on managing the fluid buildup and improving lymphatic drainage. Here’s a quick overview of what you might expect in a clinical setting: Compression Therapy Compression garments are often a cornerstone of lymphoedema management. They help reduce swelling by applying controlled pressure, which encourages the flow of lymph fluid. These garments come in different forms, including- Stocking – Sleeves – Bandages They can be custom-fitted to provide maximum comfort and effectiveness. Compression stockings are recommended to be purchased from a clinic that takes measurements of your limb and makes the stockings based on the measurements. I often refer my patients to Sigvaris in West Melbourne for these types of services.’ The benefit of this approach is that you will have a compression that is ideal for your limb, with no greater risk of fluid congestion and other side effects. Pharmaceuticals and Diuretics In some cases, medications may be prescribed to address symptoms like inflammation or to reduce fluid retention. However, it’s important to note that diuretics are generally not a primary treatment for lymphoedema, as they don’t directly address the underlying lymphatic issue. Other medications that are prescribed for Lymphoedema are creams to maintain skin moisturised in order to reduce the chance of cracking and skin damage. Manual Lymphatic Drainage (MLD) I specialise in MLD, a gentle, hands-on technique that stimulates the anastomosis of the lymphatic system and encourages the movement of excess fluid from swollen areas. MLD can be incredibly effective in reducing swelling and relieving discomfort. It works by stretching and letting the skin recoil under some really gentle pressure. This way, the lymphatic system is stimulated to work harder, and takes up the fluid to healthier parts of the body where it can be processed more efficiently. Combine Decongestive Therapy (CDT) It is part of the treatment I offer for Lymphoedema patients here at Melbourne Massage and Treatment. It consists of bandages used to compress the affected area. The compression is applied after MLD has been delivered, and it is applied to maintain fluid movement throughout the anastomosis, which is the alternative connection of the lymphatic system through which the liquid moves after the MLD stimulation. The bandages are applied and are recommended to stay on for about 24 hours. After this time, once you remove them, you will wash them, roll them and come back for another treatment. A back-to-back treatment would ensure that the swelling of the lymphoedema can be managed and reduced as quickly as possible. Laser therapy Laser therapy is a non-invasive treatment that can be used in a clinical setting to treat specific lymphoedema presentations. Indeed, Laser therapy is used when the patient already presents with fibrosis, the hardening of the skin. Low-frequency lasers are the ones used most often, and we know there are also portable pen lasers that are efficient enough for this therapy. Pneumatic compression therapy: This therapy consists of using a sleeve pump machine that gets placed over the affected area and inflates sequentially to apply pressure. The rhythmic compression helps stimulate lymphatic flow, reduces swelling, and improves circulation by encouraging the movement of excess fluid toward lymphatic drainage sites. All those therapies are recommended in combination. To start with, for the best results and quick reduction, MLD and CDT would be more effective. Surgical Treatment Options for Lymphoedema While surgery is generally considered a last resort for lymphoedema, there are certain cases where it may be necessary or beneficial: Liposuction for Lymphoedema This technique is sometimes used to remove excess fat tissue that has accumulated as a result of chronic lymphoedema. It’s not a cure, but it can help reduce the volume of swelling and improve the appearance of the affected area. Lymphovenous Anastomosis (LVA)/Bypass It involves connecting the lymphatic vessels and nearby veins, allowing excess lymph fluid to drain into the bloodstream instead of accumulating in tissues. Vascularized lymph node transfer (VLNT) a surgical technique used to treat lymphoedema by transplanting healthy lymph nodes along with their blood supply to the affected area. The transplanted lymph nodes, typically harvested from the patient’s groin or other regions, are reconnected to the recipient’s blood vessels. Lymph Node Transplantation In some specialised cases, surgeons may transplant healthy lymph nodes from one part of the body to another to help restore lymphatic drainage. This option is more complex and is usually reserved for severe, treatment-resistant lymphoedema. Surgery, of course, comes with risks and recovery time, so it is typically considered only after all other treatments have been explored. Lymphoedema Holistic Treatments: Taking a Whole-Body Approach While medical and surgical treatment options for lymphoedema can certainly help with this presentation, I firmly believe that a holistic approach is crucial for long-term success. Here are some natural and complementary therapies […]
When the lymphatic system stop working, either because for a congential malfunctioning, or because of a an external intervention, which did lead to lymphatic system damage, the individual may start experiencing symptoms of Lymphoedema. At Melbourne Massage and Treatment in Fitzroy North, Giovanni understand how challenging lymphoedema can be, which is why he provide expert care through Manual Lymphatic Drainage (MLD) and Combined Decongestive Therapy (CDT). These non-invasive treatments help manage the symptoms and improve your quality of life. What is Lymphoedema? Lymphoedema occurs when the lymphatic system is blocked or malfunctioning, leading to a buildup of lymphatic fluid. This fluid results in swelling in the affected areas, often in the arms, legs, or other extremities. Lymphoedema can be primary (a hereditary condition) or secondary (often caused by injury, surgery, or infection). The fluid that builds up in the body is a fluid that is naturally produced by the body and is released under the skin and between tissues by the bloodstream. It is reached in protein, bacteria, viruses, dust, and other minor substances that the body is unsure how to handle. Stages of Lymphoedema Lymphoedema progresses in stages, with each stage representing the severity of the condition. Recognizing the symptoms early on can help prevent the condition from advancing, so it’s important to be aware of the subtle changes in your body. Stage 0: Latent or Subclinical Stage In this early stage, there are no visible signs or symptoms of lymphoedema, but the lymphatic system may already be compromised. People in Stage 0 may experience a feeling of heaviness, discomfort, or mild swelling, int the limbs affected by this presentation, but these symptoms typically disappear after resting or with limb elevation. The fluid retention is still minimal and may not be noticed by the individual, but it can be detected through careful assessment. Stage 1: Reversible Stage At this stage, swelling is more noticeable, but the skin is still soft, and the swelling can still decrease with limb elevation and movement. When the swelling is present, the skin will feel puffy or tight, and there may be a sensation of heaviness in the affected area. In this relevant early stage, it i still easy to intervene for prevent further degeneration, and if you are unsure of what you are experiencing, reach out Giovanni for a 15 minutes free consultation, in which, at least thanks to the analysis of your clinical history, we can already evaluate if what you are experiencing is a Stage 1 Lymphoedema. Stage 2: Spontaneously Irreversible Stage In Stage 2, the swelling becomes more persistent and is not fully responsive to movement and limb elevation. The asking of the affected area may begin to feel firmer, and there can be noticeable thickening of the skin. This is the stage where fibrosis (scarring of the tissue) starts to develop, and it’s crucial to stop this from going any worse. While the swelling might fluctuate, it becomes more difficult to manage without intervention. At this point, manual treatments like Manual Lymphatic Drainage (MLD) can significantly help reduce swelling and improve the overall function of the lymphatic system. Stage 3: Lymphostatic Elephantiasis The final stage of lymphoedema is characterized by extreme swelling and thickened, hardened skin. The affected area may look large, disfigured, and become painful to the touch. Tissue fibrosis is advanced, and the skin may develop ulcerations or infections due to poor circulation and immune system function. Indeed, along with the swelling and the fibrosis buildup, the outer layer of the skin is placed further away from the blood capillary, which is responsible for releasing oxygen and other substances essential for skin regeneration.Therefore, as the skin breaks open, due to its poor condition, it is more subject to infections and contamination of pathogens. Stage 3 lymphoedema is debilitating and requires ongoing care and treatment to prevent complications and manage symptoms. At this stage, a combination of therapies such as Combined Decongestive Therapy (CDT) and MLD becomes vital for managing the swelling and restoring lymphatic flow. Common Symptoms of Lymphoedema Lymphoedema symptoms can vary from person to person and depend on the stage of the condition. The common symptoms include: Swelling: The most obvious sign of lymphoedema is swelling in the affected area, typically starting in the arms or legs. The swelling is often gradual and may worsen over the course of the day, especially after prolonged standing or sitting. Tightness or Heaviness: Affected limbs may feel heavy or tight, particularly after physical activity or at the end of the day. This sensation is often worse in the early stages and may become more pronounced as the condition progresses. Pain or Discomfort: Pain, tenderness, or discomfort in the swollen area is common, especially when there is fibrosis (hardening) of the tissues. The pain can range from mild to severe, depending on the stage. Reduced Range of Motion: As the swelling and fibrosis increase, it can lead to a limited range of motion, particularly in the arms and legs. This can impact daily activities and mobility. Skin Changes: In later stages of lymphoedema, the skin may appear thickened or leathery, with a shiny, tight appearance. There may also be visible folds in the skin, particularly around the knees, elbows, or ankles. Frequent Infections: Swollen tissues have a reduced ability to fight off infections, so people with lymphoedema are more susceptible to bacterial and fungal infections, which can further complicate the condition. Numbness or Tingling: As the swelling progresses, the nerves in the affected area may be compressed, leading to sensations of tingling, numbness, or even burning. Increased Skin Sensitivity: The skin in the affected area may become more sensitive, prone to rashes, or develop sores due to the increased swelling and poor circulation. Commonly Affected Areas of the Body Lymphoedema can affect different parts of the body, but the most common areas are: Arms: After surgery, particularly mastectomy (breast cancer surgery) that involves the removal of lymph nodes, the arms are a common site for lymphoedema. The swelling […]
Lymphoedema is a condition often associated with cancer survivors, particularly those who have undergone surgery or radiation therapy, but it can also occur due to other chronic conditions or injuries. Characterized by the swelling of limbs due to the accumulation of lymphatic fluid, lymphoedema can significantly impact a person’s mobility, emotional well-being, and overall quality of life. Early diagnosis of lymphedema and management are key to preventing long-term complications, and at Melbourne Massage and Treatment in Fitzroy North, Giovanni, a skilled Myotherapist and Lymphoedema therapist, specializes in identifying and managing this condition using a combination of manual techniques and physical assessments. In this blog, we’ll explore how lymphoedema is diagnosed, the challenges of identifying it early, and Giovanni’s approaches to detecting and managing the condition. What is Lymphoedema? Lymphoedema occurs when there is a disruption in the lymphatic system, leading to the accumulation of lymph fluid, a protein-rich fluid that sits beneath the skin and between the body’s tissue, which often causes swelling in the limbs or other areas of the body. This condition can develop due to a variety of factors, such as lymph node removal during surgery, radiation treatments, injury, or genetic predisposition. Early detection of lymphoedema is crucial to prevent the condition from worsening and causing complications like tissue fibrosis, infections, or reduced mobility. Challenges in the Diagnosis of Lymphoedema Lymphoedema can be difficult to diagnose, especially in its early stages. In its initial phase, symptoms such as heaviness, tightness, or mild swelling may seem subtle and easy to overlook. Patients might attribute these sensations to muscle strain or arthritis, delaying the diagnosis. Furthermore, swelling can fluctuate, making it even harder to identify at the outset. By the time noticeable swelling occurs, the condition may have already advanced, complicating treatment and requiring more intensive management. This is why early detection is so important, as it allows for less invasive treatments and better long-term outcomes. Giovanni’s Approach to Diagnosis of Lymphoedema As a Myotherapist and Lymphoedema therapist at Melbourne Massage and Treatment Lymphoedema Clinic, Giovanni uses manual techniques and physical assessments to diagnose lymphoedema. Although he does not use imaging technology or machines to detect the condition, Giovanni’s training and experience enable him to identify the signs and symptoms through careful observation, palpation, and physical examination. That said, if it is needed, Giovanni can write a referral doctor for your GP to indicate why he believes it is important for you to undertake a specific scan or some medical test. 1. History taking The earlier approach to Lymphoedema diagnosis is an extended look at the medical history, where any past surgery, injury, accident or medications need to be outlined and taken into consideration. 2. Clinical Assessment Following the history taken to diagnose lymphoedema is the clinical assessment. Giovanni conducts a thorough physical examination of the affected limb or area, paying close attention to key signs of lymphoedema, such as: Persistent swelling that doesn’t subside with rest Feeling of heaviness or tightness in the limb Changes in skin texture, such as hardening or thickening Reduced range of motion in the affected area Along with your booking confirmation, you would also receive a form to fill in online, which would start paving the road to your diagnosis. 3. Tape Measurement Method One of the simplest, yet effective, ways Giovanni diagnoses lymphoedema is by using tape measurements. This involves measuring the circumference of the affected limb at various points (e.g., wrist, forearm, upper arm) and comparing these measurements to the unaffected side. Over time, consistent and progressive changes in limb circumference can indicate the development of lymphoedema. While this method is cost-effective and easy to perform, it may not detect early, subtle changes in limb volume. However, when paired with other assessments, it offers valuable information about the progression of the condition. 4. The Pitting Test Giovanni often performs the pitting test, a hands-on method to assess fluid accumulation in the affected area. This simple test involves pressing down on the swollen area with his fingers. If an indentation (or “pit”) remains for several seconds after the pressure is released, it indicates the presence of excess fluid in the tissue, which is a hallmark of lymphoedema. The pitting test helps Giovanni evaluate the severity of fluid retention, but it is more subjective than advanced diagnostic tools. 5. Stemmer’s Sign – Tissue assessment Giovanni also uses palpation (manual examination through touch) to assess the affected area’s tissue texture and consistency. In the early stages of lymphoedema, the tissue may feel soft and puffy, but as the condition progresses, it can become firmer, and in some cases, the skin may develop a thicker, fibrous texture. These changes are essential indicators of lymphoedema and are crucial for determining the stage of the condition. In addition to this, the Stemmer’s Sign is a test that consists of picking what we would expect to be wrinkled skin, like the one just before the toe/tarsal joint. A positive test would result in the impossibility of pinching any skin due to the swelling in the area. 6. Lymphoscintigraphy A lymphoscintigraphy is a scan that is part of nuclear medicine tests, and it is specifically used to detect any interruption within the lymphatic system. The test is done in the specific clinic, and no recovery is needed for it. The procedure consists of injecting a radioactive liquid either in the feet or hands and with a specific camera, detecting the movement of the liquid within the body. We would expect the liquid to move within a certain timing and pathway along the lymphatic system. If that doesn’t happen, this test can give a good understanding if anything is not functioning with the lymphatic system. Why is Early Detection Crucial? The earlier lymphoedema is detected, the easier it is to manage. Early-stage lymphoedema is often easier to treat with less invasive interventions, such as manual lymphatic drainage (MLD), compression therapy (CDT), specific exercises, and skin care. These treatments can help reduce swelling, prevent the condition from worsening, and improve […]