When the space between the collarbone and first rib gets tight, during movement or even at complete rest, it can lead to Thoracic Outlet Syndrome (TOS). Between the two structures mentioned above, we have the passage of the thoracic plexus (nerves) and blood vessels. The compression of those structure, can result in pain, weakness and numbness radiating down the shoulder, arm, and hand. Because TOS has multiple causes and presentations, effective treatment depends heavily on accurate assessment and an individualised approach, and that’s where myotherapy can play a crucial role. What Causes Thoracic Outlet Syndrome? As there are different tissues passing by this space, the nature of TOS can be broadly categorised into three types: Neurogenic TOS: Compression of the brachial plexus (nerves). Venous TOS: Compression of the subclavian vein. Arterial TOS: Compression of the subclavian artery. But not only can different tissues be compressed, but different structures can be responsible for the compression. Indeed, the compression can be due to the scalene muscle, pectoralis minor or bone. And here are some common causes: Muscle imbalances that lead to poor posture (forward head/rounded shoulders); Repetitive overhead activities (which lead to constant compression of the tissues); Trauma (e.g. whiplash or clavicle fracture); Anatomical variations (such as a cervical rib). The Role of Myotherapy in TOS Assessment As a myotherapist, when treating someone with suspicious TOS, we go for a series of assessments that we compare to the clinical history and symptoms. The test itself would aim to reproduce the patient’s symptoms and guide us on what potential structure is compressed. If we are suspicious of TOS, we can aim to reduce tension in soft tissue and give exercises that can reinforce those structures to alleviate any compression in the area. Orthopedic Testing & Myotome Assessment Some common assessments include: Adson’s Test (for scalene involvement) – It consists of reproducing a drop of heart bit in the wrist (affected side) by asking the patient to abduct and extend the arm while rotating (same side) and extending the neck. This would add extra compression on the suspected structures. Roos/Elevated Arm Stress Test (to reproduce vascular or neural symptoms) – It is about asking the patient to lift the arm at 90°/90° and start closing and opening their hands repetitively for 30 seconds to 1 minute. A drop of strength or symptom reproduction would lead to a positive test. Costoclavicular Maneuver (to assess space between clavicle and first rib) – It is delivered by having the patient with depressed and retracted shoulders. The positivity of this test is given by the reproduction of symptoms or a reduction in the distal wrist. Wright’s Hyperabduction Test (for pectoralis minor tightness) – The patients get asked to lift their arm (affected side) above their head while the therapist stands behind and keeps count of the wrist heartbeat. Any symptoms, reproduction, or drop in bit is considered positive. In addition to those tests, we would use: Myotome testing: which assesses the motor function of specific spinal nerve roots; Clinical history: Any history of previous injury, surgeries, work and sport loads; Type and timing of symptoms: When and how those symptoms are reproduced on daily life. All this said, we always have to consider that as therapists, myo or physio as per osteo exc… we can assume that the positivity of many of those test leads to a positive or negative conclusion regarding TOS. Hands-on treatment and exercises in combination can be the easy steps to take to treat the presentation, but can not always guarantee the best outcome, due to each individual’s unique presentation. Hands-On Treatment and Exercise Prescription Once we have more understanding of what is potentially happening in terms of compression, a myotherapy treatment focuses on addressing the underlying causes: Manual Therapy Myofascial release of the scalene, pectoralis minor, and upper trapezius muscles. Trigger point therapy to reduce local and referred pain patterns. Joint mobilisation to improve scapular movement and rib mechanics. Neural gliding techniques to encourage nerve mobility and reduce irritation. Exercise Rehabilitation Postural re-education, particularly strengthening the deep neck flexors and lower trapezius. Scapular stabilisation exercises to improve shoulder mechanics. Breathing retraining is necessary if dysfunctional patterns (like apical breathing) are contributing to compression. Neurodynamic stretches are appropriate for nerve mobility. Together, these interventions help reduce symptoms, improve function, and support long-term recovery. The time frame for improvement, if not complete reduction of the symptoms, can be different per individual, but we can estimate a period of time that goes between 12 and 16 weeks. If no changes are reproduced within this time frame, that’s where we would refer the patient elsewhere for further investigations, like a scan. When Is Surgery Needed for Thoracic Outlet Syndrome? Surgical intervention is typically reserved for cases where conservative care fails or in cases of vascular TOS, where there’s a risk of thrombosis or embolism, but also where anatomical variations, like a cervical rib is present. Surgical procedures may include: Scalenectomy (removal of the scalene muscles) First rib resection Clavicle decompression or repair if there’s previous trauma These operations aim to create more space in the thoracic outlet, thus relieving the compression. Post-Surgical Recovery and the Role of Myotherapy In case of surgery, as a myotherapist, we can still help and ensure a correct recovery post-intervention. Treatment like MLD can help in flushing excess liquid out of the surgery area, but again, we would look into exercises as a form of recovery and rehabilitation of the area affected by the surgery and or affected by the lack of strength that is a consequence of a prolonged period of muscle weakness. More broadly, myotherapy treatment can help with: Pain management Scar tissue Muscle guarding or weakness Neurological symptoms that may persist or reappear Do You Need a Scan if we’re suspicious of TOS? Imaging, as discussed in other blogs, may be recommended when we are suspicious of other presentations, or if standard method are not creating any difference. For example: To rule out cervical disc herniation, tumours, or other causes of neurovascular symptoms. When […]
Tag Archives: muscle
Temporomandibular Joint (TMJ) disorders are a common source of jaw pain, clicking, and discomfort that can impact anyone at any age. At Melbourne Massage and Treatment in Fitzroy North, I see many clients presenting with TMJ clicking and associated symptoms. One of the key factors behind the painful symptoms is retrodiscal tissue compression, a condition that not only causes joint noises but may also lead to chronic jaw pain. What Causes TMJ Clicking? Let’s start understanding why TMJ clicks. When looking at the TMJ, we can see that between the two bones that make up the joint, there is a disk, called the articular disc, which is made of cartilage and is meant to keep the bones apart (the temporal bone and the mandibular condyle). In a healthy joint, the disc moves smoothly with the jaw during opening and closing. But when the disc is out of alignment, the condyle may snap over it, creating that characteristic “click.” For reference, a condyle is a rounded protuberance at the end of a bone, which in this case, fits into a cavity. The Role of Retrodiscal Tissue Compression in TMJ Clicking and Pain Right behind the disc lies a tissue known as the retrodiscal tissue, which contains blood vessels, nerves, and connective tissue. When the disc is displaced anteriorly, the condyle may compress this sensitive area during jaw movements. This compression can lead to: Inflammation Persistent pain Increased joint stiffness Neurovascular irritation This is possible because the tissue, as mentioned earlier, is innervated, whereas the disk is not. Therefore, the disk compression on its own is not going to replicate any pain, as there is no nerve to pick up any stimulus in there. Forward Head Posture Would Not Help. Forward head posture is a common presentation linked to TMJ clicking. Forward head posture is characterised by the head sitting forwards compared to the midline of the body, and is often due to a lack of strength in deeper neck flexor muscles. This presentation can make the TMJ presentation worse because of the excessive load placed on the muscles that surround the TMJ (masseter and temporalis muscles). Other reasons include the misalignment of the teeth, which can make the chewing action more difficult and over time, create strain along the TMJ tissues (muscles, ligaments and tendons), but also referral pain from the cervical joint tension can lead to manifest stress in the jaw and face muscle due to constant pain and discomfort. How Myotherapy Can Help At Melbourne Massage and Treatment, I offer a combination of evidence-based manual techniques and exercise therapy to address the root causes of TMJ dysfunction, aiming not just to manage symptoms but to promote long-term recovery. 1. Joint Mobilisation Gentle mobilisation techniques to the jaw, cervical spine, and upper neck can reduce joint restriction, improve mobility, and relieve the pressure on retrodiscal tissue. Mobilisation helps restore normal disc-condyle mechanics, reducing clicking and improving range of motion. 2. Dry Needling Dry needling of trigger points in the masseter, temporalis, and lateral pterygoid muscles can reduce hypertonicity and relieve pain referred to the jaw and head. Targeting myofascial restrictions can also indirectly reduce stress on the TMJ itself. 3. Targeted Exercise Therapy Specific exercises for jaw control and cervical strength are crucial for maintaining results between sessions. Jaw isometric exercises are ideal for pain management and quick relief. Resistance bend exercises for jaw opening. Relaxation techniques for parafunctional habits like clenching Over time, these exercises can enhance joint stability, reduce overloading, and in some cases improve mild degenerative changes by promoting better joint mechanics and tissue resilience. 4. Deep Tissue Massage Massaging the muscles surrounding TMJ and the cervical muscles can help reduce tension, stimulate the nervous system to relax and give a break from pain and discomfort, while improving mobility. As always, there is not one solution for the common presentation of many. Each individual is different, and the treatment results can be different. But what we can expect is that, if we balance the usage of hands-on treatment and exercises, we can create some real change with some great benefits. TMJ Clicking and Menopause Menopause is a topic I have already spoken about in my blogs. Briefly, we can refer to menopause as the period of 12 months or more of missing menstrual periods in a woman’s life cycle. Before that is called perimenopause, and after that, we talk about post-menopause. This step is achieved when a woman has no more eggs to release, and her menstruation has stopped. While it is not the same journey for each woman and there are many changes that women can go through, a common one is stiffness of ligaments. Again, this is not happening in one day, but is a change that comes with time and is different person to person. This is possible because of the lack of estrogen. Indeed, estrogen, along with controlling many other aspects of the biological life of a woman, is also responsible for the elasticity of the ligament. Put: less estrogen, less elasticity. This can explain why, during this phase, women start experiencing more TMJ pain and potentially TMJ clicking. On the other hand, we have no yet enough evidence to say that Hormonal Replacement Therapy is effective for establishing this presentation (Robinson et al., 2019). FAQ – TMJ Clicking 1. What causes the clicking sound in the TMJ?The clicking occurs when the articular disc in the jaw joint becomes displaced, and the mandibular condyle snaps over it during jaw movement. This is often due to disc misalignment. 2. Why does retrodiscal tissue compression cause TMJ pain?The retrodiscal tissue contains nerves and blood vessels. When compressed due to disc displacement, it can lead to inflammation, pain, and stiffness in the TMJ area. 3. Can TMJ clicking happen without pain?Yes. If the articular disc is displaced but the retrodiscal tissue isn’t compressed or irritated, the joint may click without producing pain. 4. How does forward head posture affect TMJ?Forward head posture strains neck muscles […]
As a Clinical Myotherapist, I often work with patients who perform back squats as part of their exercise routine, and at the question: “What’s your goal with a back squat?” the answer is often vague and not specific to what this exercise is for. The reason why the answer is not specific is simply because they don’t know what the difference is between high and lower bar squat, and don’t know that the back squat, as long as it is an amazing functional movement, doesn’t train all the lower body muscles at the same level. That’s where, to prevent injury, to perform better squats, and to strengthen more evenly all the lower body muscles, I would suggest them to do exercises like: Quads curl, Hamstring curl, Cable Machine Adduction and Diagonal Extension (Glute Medius). Back Squat: The Foundation of Strength The back squat is such a great form of exercise because it trains multiple joints and multiple muscles all at once, but also allows us to use our innate capacity of squatting, which is a functional movement, to move high loads, therefore achieving more strength gains. However, this leaves us with more responsibility to train smartly. So let’s start to break down the two main types of back squat: High-Bar Back Squat (Upper Bar Position) The bar rests on the upper traps The torso remains more upright Greater emphasis on the quadriceps muscles Ideal if your goal is quad strength and knee-dominant movement patterns Ideally, you are standing with your heels elevated from the ground The fact that the bar is sitting on the upper traps, and that the torso sits straighter, would lead to a descending movement where your back thigh (hamstrings) would lean on calf muscles, and from there you will stand back up. This is why you put more force throughout the quads. Indeed, the combination of a higher bar, a straighter torso, and a reduced descending position allows the weight to sit in the middle of the centre of gravity, which is placed more posteriorly than in a lower-bar back squat. Low-Bar Back Squat (Lower Bar Position) Bar rests lower on the rear deltoids Torso leans forward slightly more Greater load on the glutes and posterior chain Favoured by powerlifters Best for developing hip strength and glute activation Ideally, your feet are nice and flat on the ground from heel to toes. On the other hand, the lower-bar back squat, as anticipated, is more for the posterior chain muscles, like the gluteus max. This is possible because the bending forward of the trunk stretches more muscle fibres in their origin point (the posterior aspect of the ilium (the pelvic bone), the sacrum, and the coccyx), allowing more fibre contraction in the ascending movement. Also, the lower position of the bar and the bending of the torso maintain the weight in the middle of the centre of mass, which is pushed forward at this time. How about if I cannot squat deep? The depth of a squat is the distance that you can cover from a standing position to the lowest point you can reach. How deep you can squat will definitely change which muscle groups you can activate, but not everyone can squat deep —and that’s absolutely ok. Each of us has biomechanics that are different, due to differences in how the skeleton is shaped. Without going into many details in this blog, we can definitely say that those who have a longer femur would have a harder time going for a deep squat, compared to those who have a shorter femur. The femur’s length is compared to that of the torso. But this is not all, indeed, there are also other femur and hip characteristics that can limit how deep you can squat, such as an anteverted or retroverted femur head. Other conditions that can get in the way while you squat are hip impingement. Accessory Work for a Complete Lower Leg Program So, knowing when and why to use each back squat variation can help tailor your program toward specific goals or help rehab muscle imbalances through focused intent. No squat is right, no squat is wrong; it is all about your goal. However, we need to add work more specifically with other exercises for strength symmetry, muscle activation, and injury prevention. Quad Curl (Leg Extension) Isolates the quadriceps Improves knee tracking and squat depth Essential in rehab for knee pain or quad weakness Quads curl can be done in many ways, with a cable machine or on a bench with a quads curl attachment, but even with a kettlebell or resistance band. It all depends on your setup. As per all the exercises, be consistent with your set-up and progressions. What I prefer most for my training, and what I offer to my patients during the fitness class, is to do quad curls on a bench with the attachment for quad curls. The advantages of this set-up are: Confort Easy progressions Easy set-up Inclination of the back at about 45° to 65° and slight elevation of the quads. The last point is essential to ensure we engage both ends of the quadriceps femoris, which is one of the four quads, that crosses both the hip and knee joints. Hamstring Curl Focuses on the hamstrings, which during a squat are often undertrained Strengthens the back of the thigh and supports knee stability A must-have for runners and athletes prone to hamstring strains As per the quad curl, even the hamstring curl can be done with different variations; there is never one way to train those muscles, but again, it is all about the efficiency and the amount of load that we can put through the muscle, which makes a difference. And again, what I can offer at Melbourne Massage and Treatment, in Fitzroy North, is to do these exercises on a bench, using this time a lower inclination for the upper body (which is now in a prone position) so that the origin of […]
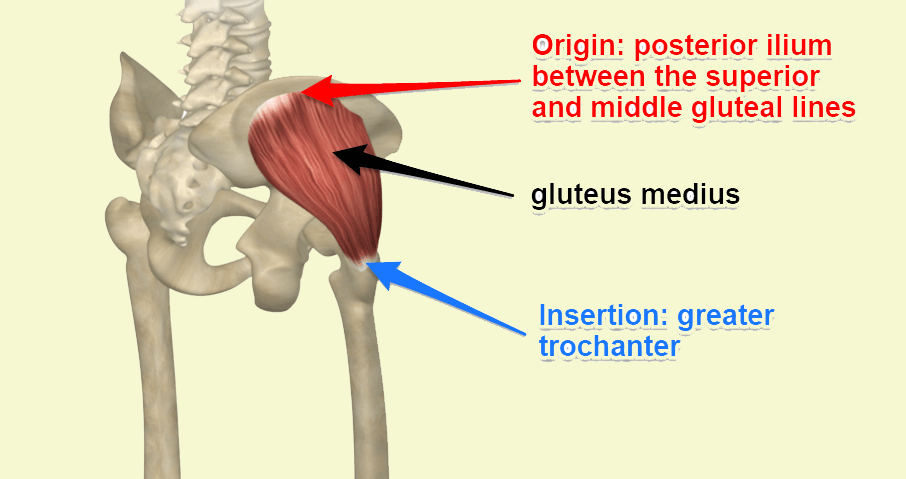
Greater Trochanteric Pain Syndrome (GTPS) is a common condition that causes persistent lateral hip pain, often making everyday activities like walking, climbing stairs, or even lying on your side difficult. GTPS primarily affects middle-aged individuals, particularly women, and is commonly linked to issues such as gluteal tendinopathy and weakness in the hip stabilizing muscles. At Melbourne Massage and Treatment, our focus is on evidence-based approaches to managing GTPS, and the latest research strongly supports the role of exercise as the first line of treatment for this condition. GTPS Symptoms Greater Trochanteric Pain Syndrome can present with a series of symptoms that are local to the side of the hip. Here are the most common: Lateral hip pain: Persistent pain on the outer side of the hip, which may extend down the thigh. Pain when lying on the affected side: Discomfort that worsens when lying directly on the hip. Tenderness to touch: Sensitivity around the greater trochanter, which may be painful to press. Pain with movement: Aggravation of pain during walking, climbing stairs, or standing for prolonged periods. Weakness in hip muscles: Reduced strength in the gluteal muscles, leading to instability in movement. Difficulty sitting for long periods: Sitting on hard surfaces can exacerbate discomfort. Mechanism of Injury for GTPS GTPS is primarily associated with tendinopathy of the gluteus medius and/or minimus muscles, with or without accompanying bursitis. As per many tendon injuries, this condition often arises from repetitive stress or overuse, leading to microtrauma and degeneration of these tendons. On the other hand, abnormal hip biomechanics can exacerbate the issue, as compressive forces cause impingement of the gluteal tendons and bursa onto the greater trochanter by the iliotibial band during hip adduction. Contributing factors to GTPS include acute trauma, such as a fall onto the lateral hip, prolonged pressure from lying on one side, and overuse from activities like running or stair climbing. Additionally, conditions like iliotibial band disorders and gluteal muscle weakness can increase the risk of developing GTPS. Understanding these mechanisms is crucial for effective management and prevention of GTPS. Evaluation of GTPS Diagnosing GTPS typically involves a combination of clinical examination and medical history assessment. After taking your clinical history, including sports and work activity, I will perform a series of tests to validate the suspicions of GTPS. Those tests include single-leg stance and resisted hip abduction, which we would expect to show weakness in single-leg standing and pain during the abduction movement. Lastly, we would also palpate the area, which is a test that is kept for last because we want to avoid flair the presentation, which may be painful with any other test after that. In some cases, imaging techniques like ultrasound or MRI may be used to rule out other conditions and confirm gluteal tendinopathy or soft tissue abnormalities. I personally do not recommend image testing as the first way to go because the impact of seeing physical damage can also have a negative impact on self-perception, making a recovery harder. At Melbourne Massage and Treatment, our focus is on evidence-based approaches to managing GTPS, and the latest research strongly supports the role of exercise as the first line of treatment for this condition. The difference between GTPS and Femoroacetabular Impingement (FAI) The difference between GTPS and FAI stands in the hip area involved in the injury. The GTPS is relative to the side of the hip and involves the gluteus medius and minimus tendon and the bursa that separate that tendon from the greater trochanter of the femur. On the other hand, FAI is a presentation that still involves the hip, but it does take place on the anterior portion of the hip, as is characterised by and overgrowth of tissue on the femur head or the hip socket, and it does manifest with hip flexion and external rotation. That’s why it is important to receive an evaluation of the presentation from a professional, in order not to mix the two presentation, or also, in order to evaluate if both presentation are present at the same time, which can also happen. The Role of Exercise in GTPS Treatment A recent systematic review and meta-analysis analyzing multiple randomized controlled trials found that structured exercise provides significant benefits for individuals with GTPS. The findings revealed that: Long-term pain reduction: Exercise can lead to slight but meaningful reductions in hip pain over time. Improved physical function: Patients who engage in targeted exercise programs experience better mobility and overall hip function. Increased likelihood of meaningful recovery: Compared to corticosteroid injections, exercise significantly increases the chances of noticeable improvement in symptoms. One of the most notable takeaways from this research is that exercise has a long-lasting effect, whereas treatments such as corticosteroid injections may provide only short-term relief. Additionally, no serious adverse effects were reported with exercise-based interventions, making it a safe and sustainable approach to managing GTPS. Why Choose Exercise Over Corticosteroid Injections? Corticosteroid injections have often been used for GTPS pain relief, but the research indicates that exercise leads to better long-term outcomes. While injections may offer temporary symptom relief, they do not address the underlying causes of GTPS, such as gluteal muscle weakness or tendon dysfunction. Exercise, on the other hand, strengthens the hip muscles, improves joint stability, and reduces the likelihood of recurring pain. In a previous blog post, I spoke about the key role of Gluteus Medius as a pelvis stabiliser. Effective Exercises for GTPS At Melbourne Massage and Treatment in Fitzroy North clinic, I design individualised exercise programs to help patients with GTPS regain strength and function. Some of the most effective exercises for GTPS include: Isometric exercises involve holding static positions to engage the hip muscles without excessive movement, reducing pain and improving muscle endurance, driving blood to the tendons and joints, helping with recovery. Strength training: Progressive strengthening of the gluteus medius and minimus muscles to enhance hip stability. Functional movement training: Exercises that mimic daily activities to help improve movement patterns and prevent pain triggers. Along those exercises […]
When it comes to maintaining a healthy, functional body, it’s easy to overlook the pivotal role of certain muscles in everyday movement and long-term stability. One such muscle is the gluteus medius. At Melbourne Massage and Treatment, located in Fitzroy North, I see many patients who either love running or love to hit the gym but are not aware of the importance of this muscle for their activity. What is the Gluteus Medius? The gluteus medius (GM) is one of the three primary muscles of the gluteal group, located in the upper part of the buttock. Here is a breakdown of its anatomy: Origin: the gluteal surface of the ilium Insertion: lateral surface of the greater trochanter Innervation: dorsal branches of the L4, L5, and S1 Actions: Abduction and medial rotation of the lower limb. It stabilises the pelvis. Thanks to its positioning, the GM plays a vital role in controlling pelvic movement, specifically in the stabilization of the pelvis during various motions like walking, running, or standing on one leg. More Information About Gluteus Medius actions The GM serves several essential functions that directly affect the stability of the hip and lower body: Pelvic Stabilization: One of its primary roles is preventing the pelvis from tilting excessively to one side when you move, especially when you’re walking or running. If the gluteus medius isn’t working properly, the opposite side of your pelvis may dip downward, leading to an imbalance and compensatory movements that strain other parts of the body. Hip Abduction: The gluteus medius helps to move the leg out to the side, away from the body. This movement, known as hip abduction, is crucial for activities that require lateral movement, such as stepping sideways or maintaining balance while performing physical tasks. Internal and External Rotation: The gluteus medius also assists with the rotation of the hip joint. Depending on which fibers are activated, it helps with both internal and external rotation of the thigh. This is essential for maintaining control and precision in movements. Postural Support: The gluteus medius muscle helps keep the pelvis level when you’re standing on one leg. Without proper activation of this muscle, one hip might drop, affecting posture and causing misalignments in the spine and lower back. The Role of the Gluteus Medius in Hip Stability Why is the GM so important for hip stability? Simply put, this muscle acts as the stabilizer of the pelvis. Without a properly functioning gluteus medius, other muscles and joints are forced to compensate for the lack of stability, leading to overuse and strain. For example, improper GM function can result in excessive stress on the knees, lower back, and even the ankles, which can lead to pain, discomfort, and injury. Clinical implications are vast, especially for athletes and individuals who regularly engage in physical activities. Hip instability can result in difficulty performing simple tasks like walking or climbing stairs, and over time, it may contribute to chronic conditions such as hip osteoarthritis. A common painful presentation that we see in athletes but also the everyday patients is Greater Throcanta Pain Syndrome (GTPS), which is characterised by the side hip pain. This presentation results from a GM tendon irritation. Signs of Weak or Dysfunctional Gluteus Medius Here are some common signs that your gluteus medius may need attention: Pain in the hip or lower back: Since this muscle is integral to proper alignment, dysfunction often manifests as discomfort in the hips or lower back. Difficulty balancing on one leg: Struggling with stability when standing on one leg may indicate weak gluteus medius muscles. Shifting or limping while walking: A noticeable shift or limp while walking can point to weakness in the gluteus medius, causing the body to compensate and disrupt your gait. How can Gluteus Medius impact your run? The gluteus medius is crucial for runners as it stabilizes the pelvis, controls hip movement, and ensures proper alignment during running. This muscle prevents excessive pelvic tilting, reduces side-to-side sway, and helps maintain efficient running form, thereby lowering the risk of injuries such as knee pain, IT band syndrome, and lower back discomfort. A weak or dysfunctional gluteus medius can lead to compensatory movements, affecting performance and causing imbalances. How Melbourne Massage and Treatment Can Help At Melbourne Massage and Treatment, as a clinical myotherapist, I focus on treatment designed to address muscle pain and dysfunction through a variety of techniques. One of the key areas of focus is to create a treatment plan that works for your presentation based on your clinical history. Here is a breakdown: 1. Assessment and Diagnosis: I would conducts a thorough assessment to identify if the gluteus medius is underperforming, weak, or compensating due to other musculoskeletal issues. This involves a combination of posture analysis, movement patterns, and targeted strength tests. 2. Myotherapy Treatment Techniques: I will use various techniques, including trigger point therapy, Dry Needling, myofascial release, and deep tissue massage, to release tension in the gluteus medius and surrounding muscles. This helps to restore proper function, reduce pain, and improve mobility. 3. Rehabilitation and Strengthening: After addressing any issues, we will work to develop rehabilitation strategies, including targeted strengthening exercises for the gluteus medius and other muscles that surround the pelvic, lower back and leg area. These exercises aim to restore proper muscle activation and prevent future imbalances. 4. Injury Prevention: In order to prevent further injury, we will set a target of strength that you want to achieve with your sports activity, and we will do our best to hit that target. Be mindful that based on your presentation, the target could extend from a few weeks to several months. The Takeaway The gluteus medius muscle is far more important for hip stability than many people realize. Its role in maintaining pelvic alignment and controlling movement is essential for pain-free mobility, proper posture, and long-term musculoskeletal health. Whether you’re dealing with hip pain, experiencing difficulty with balance, or want to prevent future issues, understanding and caring for […]
A deadlift (conventional deadlift) is a popular exercise that aims to strengthen your posterior chain muscle, including the erector spinae muscle, glutes, and hamstring. It is considered a really top list of important exercises to do, and it can be fun and rewarding, but when the weight you move starts increasing, it can lead to severe injuries if you are not using the right technique. Let’s then look into what we need to do to get a good deadlift by starting to analyse from bottom to top how the body should be placed. Centre of mass and biomechanics in deadlift To start with, let’s talk about the biomechanics and the centre of mass for a deadlift. When doing exercises, biomechanics plays a crucial role in safety and optimal exercise execution, and there is no exception for the deadlift. Furthermore, along with all exercises, the lifting and the descending part, the weight has to be in line with the centre of mass. These two components are strictly interconnected to the other one, which means if I don’t use the right biomechanics, I am not going to have the weight aligned with the centre of mass, or if the weight is not aligned with the centre of mass, I am not using my biomechanics at its full potential. So, what’s the centre of mass in the deadlift? The centre of mass in a deadlift is that imaginary line that runs right from the mid-portion of your feet up right in front of your shins, and as you lift the weight up, it passes right in front of your pelvis. That’s where the bar is going to end once you complete the lifting motion. What happens if I don’t keep the bar along the centre of mass? At any stage, during the lifting or the descending motion, if you move the bar further away from the centre of the mass line, there is a great danger of injury. This is because, as the weight travels away from the centre of mass, there is an increase in momentum, which means that your muscles and ligaments that are working hard to move the weight are suddenly placed under a greater load. What are then the proper biomechanics to observe along a deadlift? Ankle and Knee To execute a good deadlift, we want to ensure we have good ankle dorsiflexion, which is not as important as when we squat, but still, we better ensure it is working right. This would allow a straight forward movement of the knee, which would not need to find its way medially or laterally along the initial bending for when we go to grab the bar. Moving up the chain, as we said, the knee have to point straight ahead, following the toes direction. Hip and lower back Next is the hip. This is an important joint, and here is where we need to make sure that we tilt the pelvis forward (bring the teil bone upwards) and as we hinge the hip, we have to have enough movement in there that the greater trochanter (bone landmark that represents the side of the femur’s head) is posterior to the malleolus (the bone landmark that make the side and medial portion of the ankle). Now, if we managed to have tailbone project far back and up, and hip hinged with a slightly bent knee, our back up to cervical area would be alrady quiet flat. Thoracic and head If we keep going upwards, we get to the upper thoracic area, right between the scapula. Here, we want to keep the scapula protracted and have the rhomboids and serratus anterior muscles active and strong so that the arms can hang down straight towards the bar and sit right next to the knee. Regarding the head, use your eyesight to look down at the floor at 45° in front of you and feel the ears pulling away from the shoulder. That would keep your neck nice and long and place the head in the right position. Arms and hands Arms hang down from the shoulder in a straight line, from the AC Joint down to the wrist. The arm has to feel heavy and prolonged, and the hands must sit right next to the shin. Indeed, your arms must stay as wide as your shoulders. That would ensure that your arms are at 90° with the bar, and from a vertical pool point of view, they can take the maximum load ever. Lastly, regarding the hands, there are different grip types that can be used for the deadlift. What is most important is that the wrist is straight following the armline. For exercise purposes, you can have a regular grip where your thumb is gripping around the bar. For heavier weights, you may want to do a mixed grip, where one hand (the dominant one) has the palm facing forward, and the other hand has the palm facing you. In conclusion, the biomechanics of the deadlift, if used correctly, will allow you to always weight in a safe spot, in line with the centre of mass. Your back has to be flat at all times, and along the exercise execution, you want to grasp air in, engage the core to flat out the lower back and then you can lift off. Benefits of Deadlifting Now, let’s look into the benefits of deadlifting. Full-body workout: Deadlifts engage multiple muscle groups—glutes, hamstrings, quads, lower back, core, traps, and forearms—providing a full-body workout in a single movement. Improved strength: Deadlifts are among the best exercises for building overall strength, especially in the posterior chain (back, glutes, and hamstrings). Better posture: Deadlifts can improve posture and reduce the risk of slouching by strengthening your back and core muscles. Core stability: The movement requires significant core activation, helping to enhance core strength and stability. Increased athletic performance: Deadlifts translate well to other athletic movements, as they improve explosiveness, agility, and endurance. Fat loss: The intensity and demand on […]
In the world of fitness and wellness, stretching has long been hailed as a crucial component of any exercise regimen. But what if we told you that the benefits of traditional stretching might not be as clear-cut as we’ve been led to believe? At Melbourne Massage and Treatment in Fitzroy North, we believe it’s essential to examine the science behind standard practices. Let’s dive into why the traditional notion of stretching might be more myth than fact. The Stretching Paradigm For decades, stretching has been touted as the go-to method for improving flexibility, preventing injury, and enhancing performance. From pre-workout rituals to post-exercise cooldowns, the idea is ingrained in our fitness culture. However, recent research suggests that many of these beliefs may lack substantial scientific backing. Limited Evidence for Injury Prevention One of the primary arguments for stretching is its role in preventing injuries. Yet, numerous studies have indicated that static stretching (holding a stretch for a period) before exercise may not effectively reduce injury risk. In fact, some research shows that static stretching can temporarily weaken muscles, potentially leading to decreased performance, especially in sports requiring strength and power. Flexibility: A Double-Edged Sword While flexibility is important, excessive stretching can sometimes lead to hypermobility, which can be just as problematic as tightness. Hypermobile individuals may experience joint instability, increasing their risk of injury. Instead of focusing solely on stretching, a balanced approach that includes strength training and stability work may offer a more effective solution. The Case for Dynamic Movement Instead of traditional stretching, consider incorporating dynamic movements into your warm-up. Activities like leg swings, arm circles, and bodyweight exercises can effectively prepare your muscles for activity without the potential drawbacks of static stretching. Dynamic movements increase blood flow and activate muscles, leading to better performance without the risk of overstretching. If you are not sure what movement fit your needs, think about what exercises or sports acitiviy you are about to perform. An example would be a soccer match. Soccer involve running, quick change of direction, hip flexion and more lower body work. So what about doing some calf raises to warm up your calf muscles, which are going to be ready to make your run? Go for some squats that can focus on glute activation and quods activation, based on the type of squat that you are performing. Lunges that would ensure your quods warm up and your knees take some load. Plyometrics are a good way to warm up, too, such as skipping the rope or explosive squat. The Role of Massage and Other Therapies At Melbourne Massage and Treatment, we emphasize the benefits of massage therapy, myofascial release, and other treatments that promote muscle recovery and relaxation. These techniques can enhance flexibility and range of motion without the risks associated with excessive stretching. By addressing muscle tension and improving circulation, these therapies can provide a holistic approach to wellness. Tendons and Ligaments: The Stretching Sensitivity Tendons and ligaments are essential components of our musculoskeletal system, providing stability and support to our joints. Unlike muscles, which are designed to stretch and contract, tendons and ligaments are less pliable and don’t respond well to excessive stretching. When stretched beyond their natural limits, they can become overstressed, leading to micro tears or even injury. This lack of elasticity is why it’s crucial to approach flexibility with caution—overstretching can compromise the integrity of these structures, increasing the risk of strains and sprains. Instead of focusing on prolonged stretching, prioritizing strength and stability can help maintain healthy tendons and ligaments, ensuring that your body remains resilient and injury-free. What indeed our tendons and ligaments prefer as a form of activation are the isometric exercises. Conclusion While stretching may have its place, it’s crucial to question its effectiveness as a one-size-fits-all solution. Instead of defaulting to stretching, consider a more integrated approach that combines dynamic movement, strength training, and bodywork therapies. At Melbourne Massage and Treatment in Fitzroy North, we’re here to help you develop a personalized plan that prioritizes your health and well-being, and to start your journey book now a 15 minf free consultation for a treatment plan. Remember, wellness isn’t about following trends; it’s about finding what truly works for your body. Let’s move beyond the myths and embrace a more science-backed approach to fitness and recovery. FAQ Q: Why has stretching been considered important in fitness for so long? A: Stretching has been viewed as essential for improving flexibility, preventing injuries, and enhancing athletic performance, leading to its widespread adoption in pre- and post-workout routines. Q: Is there scientific evidence supporting the claim that stretching prevents injuries? A: Recent research indicates that static stretching before exercise may not effectively reduce injury risk. In fact, it can temporarily weaken muscles, potentially decreasing performance, especially in strength and power sports. Q: Can excessive stretching be harmful? A: Yes, excessive stretching can lead to hypermobility, which may cause joint instability and increase the risk of injury. A balanced approach that includes strength training is often more beneficial. Q: What are dynamic movements, and why are they preferred over static stretching? A: Dynamic movements, such as leg swings and arm circles, effectively prepare muscles for activity by increasing blood flow and activating muscles. They help improve performance without the drawbacks associated with static stretching. Q: How can I warm up effectively for specific sports? A: Tailor your warm-up to the activity. For example, before a soccer match, you might include calf raises, squats, and lunges to activate the necessary muscle groups and prepare your body for movement. Q: What role does massage therapy play in fitness and recovery? A: Massage therapy and myofascial release enhance muscle recovery and relaxation, improving flexibility and range of motion without the risks of excessive stretching. Q: How do tendons and ligaments respond to stretching? A: Tendons and ligaments are less pliable than muscles and can become overstressed when stretched excessively. This can lead to microtears or injury, making it important to approach flexibility with […]
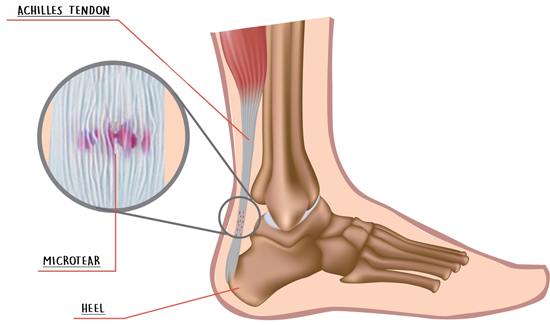
Achilles tendinopathy is a condition that manifests on the lower portion of the calf and is caused by overusing the muscle of this region, such as Gastrocnemius and or Soleus. Initially, you may not notice the issue, as it starts as a low-level inflammation and micro-tearing, but as the condition progresses, the damage and inflammation become more relevant. Achilles Tendinopathy can be easy to treat and manage when treatment is delivered in the early stages. If the injury is not looked after, the occurring damage could be much harder to resolve. Symptoms Most commonly, people experience pain in the morning or when the muscle is still cold. As the day progress and you start moving around, the pain may dissipate, and you start feeling better, ignoring the danger. Occasionally, the area would present swollen and or tender at the touch. Treatment options for Achilles Tendinopathy The management of this condition starts by improving the rest time and time off from sports activities, such as: Running Soccer Any sport which includes jumping or being on feet Other helpful approaches include: Heat pack Dry needling Improving Ankle and Big toes the mobility Massage Therapy Rock taping Achilles tendinopathies are not a condition that will heal on its own. As mentioned, it will feel better with rest, but as soon extra activities are played, the pain can back as strong as. Remedial Massage and or Myotherapy treatment can help target the painful area, stimulate an immune system response, and help with the recovery process. Also, along with the hands-on deep tissue work, mobilisation is a great way to reduce the tension in the ankle joint and improve the muscles’ functionality. After treatment, Giovanni will give you some exercises to take home. Those exercises would keep the area tension free, improve the joining mobility and strengthen the area.
Myofascial Dry Needling (MDN) treats sore muscles and trigger points. How does Dry Needling work? As discussed in another blog post, muscles are made of many individual fibres. As the fibre contract and stretches, this does give the muscle the ability to have strength and elasticity. Along with repetitive movements and lack of posture, the muscle fibres can accumulate tension that we generally call knots. Those “knots” are also known as trigger points. This is one of the many theories behind the formation of trigger points. Said so, a trigger point is a terminology used to describe a painful spot. And still, nowadays, there is no exact explanation for how trigger point forms and what exactly they are. But what we know for sure is that not everyone develops trigger points in the same spot. Now, to release the tension out of the trigger points, we can either apply external pressure, with the thumb or the elbow, in case of a Remedial Massage or even the knee or the heel of the foot with a Thai Massage, or we can break the fibres from within by using a needle. What a needle is like? The needles used in this practice have a diameter from 0.15 to 0.25mm, so really thin needles. Whereas the length can vary from 15mm to 90mm. Depending on the target muscle, the length of the needle is different. So, as we penetrate the muscle with the needle, we brake the fibre, and we recall an inflammatory response from the patient’s immune system. Which drives more blood and nutrients to the target area. As discussed further in this study published on PubMed, Dry Needling is effective for chronic non-specific neck pain 1. Is dry needling safe? Yes, it is, as long as the practitioner offering the service is qualified for it, and well knows the anatomy of the muscles. Said so, when you receive dry needling, there are a few things that you may want to consider. Firstly you better not have any metal allergy. Also, Dry Needling is not recommended if you have just done any strong physical activity or training, as the muscles would be in an acute inflammatory stage. In addition to this, other contraindications are: If the patient is on a blood thinner Diabetes type 1 The area is affected by Lymphedema The patient is unable to give the consent The patient would not be able to stay still as the needle is in the body Book now, your next Myotherapy session at Melbourne Massage and Treatment, Fitzroy North Clinic. How long the needle stays in the body? Depending on the area needing treatment, the needle may stay in the body for 3 to 10 minutes. And always based on the target muscle that needs to be treated would also depend on the type of treatment. Indeed, the needle could be placed in the muscle and left there to sit and create the physiological response needed, or it could even be partially extracted, moved around and placed back. This type of technique is called “peppering”. Peppering along a dry needling session allows the therapist to target other fibres around the muscle fibre area. 1. Cerezo-Téllez E, Torres-Lacomba M, Fuentes-Gallardo I, Perez-Muñoz M, Mayoral-Del-Moral O, Lluch-Girbés E, Prieto-Valiente L, Falla D. Effectiveness of dry needling for chronic nonspecific neck pain: a randomized, single-blinded, clinical trial. Pain. 2016 Sep;157(9):1905-1917. DOI: 10.1097/j.pain.0000000000000591. PMID: 27537209.
Muscle and Tendon are two types of fibres that connect bonds, allowing the joint to be moved by contracting or extending. Muscles and Tendons characteristics. A muscle consists of fibres of muscle cells covered by fascia, bundled with many more fibres, surrounded by thick protective tissue. So each muscle fibre is covered in the fascia, then wrapped as a whole muscle in more fascia. A tendon is a high-tensile-strength band of dense fibery connective tissue. Indeed tendons can transmit the mechanical forces of muscle to the skeletal system. Tendons, as per ligaments, are made of collagen fibres. Compared to a tendon, a muscle is elastic and sits in between 2 tendons parts which keep the muscle itself connected to bonds. So yes, muscles are not directly connected to bond themself. Luckily, there is to say, because if this was the case, it would be really easy to suffer from injuries like a muscle tear. Said so, it is now easy to understand that tendons are capable of holding more force. Injury type Due to the consistency of the tendon and its functionality, we can now understand why a tendon tear or rupture is a severe injury that requires surgical intervention and months of rehabilitation. On the other hand, often, after months of rehabilitation, still, the tendon would not go back to its original state. A common tendon rupture is Achille’s tendon. Achille’s tendon connects the lower part of the Gastrocnemius and Soleus to the foothill. Repetitive movement and repetitive partial load on this tendon are the leading cause of injury. Healthy muscle and tendon Simple and gentle exercises are a good way to keep your muscle and tendon out of trouble. The key points of these types of exercises are: Consistency Resisted load (by using rubber bands) Starting with light weight to then building up with time heavier load Good posture doing the exercises Have a day of rest from exercises once a week Avoid exercises that aggravate your pain. Said so, other critical points for muscle and tendons good health seating into: Having a good night’s rest Eating more fresh food than overprocessed food Regarding recovery from an injury, as previously mentioned in the ice pack and/or heat pack posts, the usage of temperature is recommended based on the stage of the injury and the pain experienced with it. Even though on an inflamed tendon, never apply a heat pack. Are you in need of treatment? Don’t look any further, and book your initial consultation by clicking here.
- 1
- 2