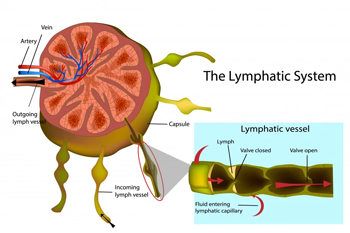
A surgery is an invasive procedure that involves cutting your skin open to intervene on your musculoskeletal system and or the organs. Surgeries are often a life-saving intervention, but even a life-changing intervention. Once you undergo surgery, your body will never be the same. MLD post-surgery can help stimulate your Lymphatic System, supporting your recovery from this type of intervention. The lymphatic system is a body system that collects, moves and cleans the excess water and substances, like bacteria, viruses, dirt, tattoos, ink and more, from below the skin and then passes it to the bloodstream. Lymphatic System and Surgery. 80% of the Lymphatic System sits below the skin, and 20% sits within the deep fascia. When going for surgery and the skin gets cut, the superficial layer of the lymphatic system gets interrupted and is damaged. Unless we intervene, the lymphatic system will have a hard time regenerating. Indeed, the lymphatic system can regenerate if stimulated. The stimulation of the lymphatic system happens through touch, like with MLD or through the movement of the body, like exercises, even as simple as muscle contraction. MLD Post-Surgery – How It Works? Before or after surgery, it is recommended to stay active. This would allow the different body systems to keep working and maintain their function at their best till the time of the surgery. On the other hand, being active post-surgery is not always an option. In fact, during the post-surgery period, being active in the area that got stitches can be a contraindication, as the stitches could break. A cast may be present in other cases, and the muscle near the surgery can’t be moved. That’s where MLD can help stimulate the lymphatic system. By doing so, we can guarantee the circulation of liquids in the body, which is essential for a great recovery. But not only that Reducing the swelling around the cutting area or below the area affected by the operation would guarantee a fast return to movement. This is because the less swelling, the easier it is to move the joint. But also, MLD comes with a deep relaxation effect, which would put you in a state of relaxation and would help you move more easily. So MLD, by boosting the lymphatic system, reduces the swelling and allows the body’s natural healing process. What to do if you have to go for surgery then? If you are up for surgery soon and you have no contraindication to MLD, what you can do to guarantee a faster recovery is, keep moving as much as you can, stay active, and book yourself in for a few MLD treatments just for the days before your surgery is due. That would help with the Lymphatic System recovery, as a more robust and healthier Lymphatic System would recover faster. And as the risk of infection and post-surgery is under control, and your blood pressure is within the acceptable range (this depends on what type of surgery you had), get moving as much as possible and come back for a few more sessions of MLD. MLD post-Surgery – Does It Work For Any Surgery? C-section (preeclampsia) bone fracture liposuction carpal tunnel knee reconstruction hip replacement day hospital intervention MLD Post-Surgery – What You Should Know As often happens with cancer surgery, lymph nodes get removed if they are contaminated by cancerous cells. After surgery, you may also be treated with chemotherapy or radiotherapy in the area affected by the surgery. Lymph node removal prevents the cancer cells from spreading throughout the rest of the body, so it is often an inevitable step in this type of intervention. The risk of developing lymph node removal, on the other hand, is represented by the development of Lymphoedema after a cancer surgery, which depends on many different factors, including lifestyle, genetics, radiation therapy and more. I dedicated a series of blogs to the Lymphoedema topic, which you can find here. On the other hand, If you are concerned about Lymphoedema presentation, get in touch now to discuss how Giovanni can assist you. Giovanni’s Training For MLD I trained for MLD on two separate occasions with the Vodder Academy, whose courses in Australia are offered by Moving Lymph. The first course I did was in 2021, and I trained to work on patients who had an intact lymphatic system. My training was already complete to work with patients who undergo surgery. It was then in 2024 that I took a course for Lymphoedema therapy. This second had a strong focus on conditions where the lymphatic system is interrupted. Either because of a congenital presentation (primary lymphoedema) or because of external intervention (secondary Lymphoedema). FAQ – MLD post-Surgery
Tag Archives: therapeutic
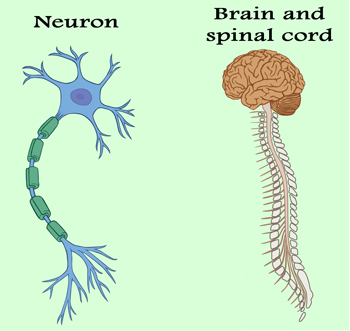
The Nervous System (NS) controls the voluntary and automatic functions of the body. It is made up of: brain spinal cord nerves Subdivision of the Nervous System The nervous system, initially, can be divided into the Central Nervous system (CNS), which is made of the Brain and Spinal Cord and the Perhiperic Nervous System (PNS), which consists of nerves that connect the CNS to the rest of the body. In more detail, the PNS can be divided into Sensory Neurons and Motor Neurons, the Motor Neurons can be divided into Somatic Neurons and Autonomic Neurons, and finally, this last is divided into the Sympathetic and Parasympathetic Nervous Systems. The function of the Nervous System The nervous system can also be defined by its functionality. For this subdivision, we have three categories: Sensory Affarent function Integrative function Motor Efferent Function The afferent function is characterised by a signal that travels to the brain from the PNS. The integrative part analyses the sensory information, stores some aspects, and makes decisions regarding appropriate behaviours. The Motor does respond to the stimulus by initiating an action. The Nervous System is made of Neurons. Neurons carry messages to and from different parts of the body. To be functional, neurons need three components: Oxygen Stimulation Food Neurons can start within the brain and travel down to the spine or can begin with the peripheric portion of the body and travel to the spine and brain next. Either way, the information can travel in one direction only. For afferent neurons, the direction is from the peripheric body portion to the brain, and the efferent is from the CNS or Brain to the peripheric part. Synapses connect neurons. The Synapse is the space where information is exchanged between two neurons. For a signal to be transmitted along a neuron, a chemical reaction has to happen within the neuron cell. This chemical reaction is better known as Action Potential. Once an Action Potential is started, an electric signal, within the order of mV would be transmitted from the Neuron cell to the opposite end, called Axon Terminal. At The Axon Terminal, the neurotransmitter would be passed and sent to the next neuron, receiving those substances through the receptors on its cell membrane. This is just a simplification of how communication between two neurons happens. In reality, there are variations to this communication methodology, and not always does the communication succeed. The NS is responsible for the following: memory, learning and intelligence movement controls the organs’ functions: – heart beating – breathing – digestion – sweating the senses: – sight – hear – taste – touch – smell The Sympathetic and Para-Sympathetic NS. The Autonomic NS controls the body parts we don’t have to think about it, like breathing, sweating or shivering, indeed the main organs. The SNS controls how we respond to emergencies. It makes our heart beat faster and causes the release of adrenaline. Where the parasympathetic nervous system prepares the body for rest (for example, when we go to sleep). The PSNS and the SNS work together to manage the body’s responses to our changing environment and needs. Massage and Nervous System As massage or manual therapy is a direct stimulus of the body, it plays a role in the response of the NS. What can happen is due to genetic factors, muscle tensions, and bulge disk nerves can get trapped along the way. Using the different testing approaches, such as Myotome and Dermatome, Giovanni can guide you through understanding where the nerve got entrapped or pinched. But this type of work is mainly for conditions where physically the nerve is involved in pour functionality. An example can be when someone has poor strength, on one hand, compared to the other, or when the sensitivity of a patch of skin is not so accurate. MLD and Nervous System Another technique, such as MLD (Manual Lymphatic Drainage), plays a role in the Parasympathetic Nervous System. An MLD treatment is profoundly relaxing, as it calms the nervous system, reduces pain and restores balance. This happens because of the mechanic repetitive movement used during the technique. There for, no pain has to be replicated during the treatment, or the SNS gets activated, as per pain response, and the body goes into “alarm” mode. Physical or mental pathologies can play a crucial role in the functionality of the nervous system, and techniques like MLD or Massage therapy generally can help in reducing symptoms and assisting in overcoming pain and body dysfunctions. Along the mental conditions, we find Anxiety or Depression too. In conclusion, any Massage Therapy or Manual Therapy, including Thai Massage, Remedial Massage, MLD and or Myotherapy, are great tools to release the tension in the body and improve the status of the nervous system. On the other hand, breathing, as per already disgust in the breathing wave blogs (Blog 1, Blog 2) plays a vital role in the well-being of the body, mind and nervous system. Feel stressed and need to release some tension? Book now your next massage at Melbourne Massage and Treatment.
On the occasion of my 4th time in Chiang Mai, since 2018, I am dedicating this post to Thai Massage in Pichest Boonthumme Style. When and where did it all start? In March 2018, I started studying and practising Thai Massage. I came here to Chiang Mai, to see Pichest Boonthumme, after a friend’s recommendation. I was looking into finding someone, that could teach and share a massage technique, not only based on sequence and repetitive movement. As often happens, as long as you ask, what you are looking for will show up. And now, after 3 long years of the Covid pandemic and limitations on travelling, I am back in Chiang Mai. This is my first trip out of Australia since 2019, so it was an excellent way to celebrate the freedom of travelling, once again. Being back at Pichest Thai Massage School is always challenging. Even though I spent the last three years training for Remedial Massage, Myotherapy and MLD, when I came here, there was always something new to learn. Along with that new practice, there is always the Thai/Buddhist philosophy aspect of how to see things. I did really like the way Pichest, with his limited English, can explain the complex way life can present and shape, and how simple it is to learn how to deal with it. Just observe the breath. Well, no surprise, as this is the principle of Vipassana Meditation itself. That said, what most often happens is that people who come here to study with Pichest ask to learn how to breathe, even before they can receive a massage. Many people come here because they heard of how good Pichest is at giving massages. And they all come with the expectation to get fixed. And it is just hilarious to see how Pichest, every time, turn these people away from treatment and asks them to learn how to breathe. We are used to thinking of Thai Massage as a painful approach, a strong technique, and it is. But not because we are physically suffering means we are getting better. If we can’t deal with the pain if we stop breathing as we perceive that pain, we keep creating tension in the body and will not let the healing process happen. Breathing during a massage comes with a series of benefits: helps the blood to be pushed around Oxygenation of the muscle tissues Improve relaxation It helps in dealing with the pain reproduced by the touch of a tense area Stimulates the Vagus Nerve, which controls the parasympathetic nervous system On the other hand, before we start doing deep work on the body, the patient does better take 5 minutes to practice breathing, and the first area to work would be around the posterior portion of the shoulder and the hip or Tibia area, to stimulates the blood flow within the body. In conclusion, Thai Massage as we know it in the West is a bit of a distortion of the real thing. Thai Massage, as with any deep tissue massage, can replicate pain, but the pain must be good, not sharp. The pain must help to release tensions and not increase them. And to be a Thai Massage therapist, you better know your anatomy well. Are you curious to find out what a traditional Thai Massage is like? Bookings are open for Traditional Thai Massage at Melbourne Massage and Treatment Fitzroy North studio.
Mobility is the degree to which a joint can move before being restricted by surrounding tissues. Not all the joints taught are considered mobility joints. The Mobility and Motility Joints Theory Starting from the big toes joint and moving up the body to the upper cervical joints, we can count one by one a mobility joint alternating with a stability joint. So this would be like this: Big toes – M. Metatarsal – S Ankle -M Knee – S Hip – M Lumbar -S Toracic – M Lower Cervical – S Upper Cervical – M Shoulder – M Elbow – S Wrist – M Tarsal – S Fingers – M The major differences are: A Muscular structure surrounds mobility joints Stability joints are surrounded by ligaments and tendons Mobility joints move in more planes than stable ones. The stability joints, indeed are essential to the body mechanics to ensure that gravity and force applied to the body by its own weight are well distributed. First thing first. Now, if we plan to strengthen our body, like by going to the gym, running or doing any sports activity, ideally we would like to ensure that the mobile joints can deliver the minimum required of ROM. Why? Well, if the mobility joints are stiff or not mobile enough, the priority of moving would not diminish and the stability joints, are going to do their best to compensate. But let’s see this with an example. Mark (name of fantasy) who is an office worker, spends about 40 hours a week at his desk, and to reduce the work and life stress decided to start a routine run 3 to 4 times a week for 1 hour per time. Mark thinks that to go for a run, you don’t need training and has no clue about the mobility, stability and strengthening chain. After a few weeks that is enjoying his new routine, Mark start experiencing knee pain. Mark also didn’t realise that due to the long hours of sitting at the office, his hips joint are tight, and his external rotators, such as the gluteus max and piriformis, are tight. As per consequence, when Mark stands up, the angle of the gate (AOG), which refers to the rotation of the foot in a standing position, is up to 4 toes per side. (3 toes is the max AOG we expect in the foot). Now, what happens next is that when Mark goes running, his ankle mobility and hip mobility are visibly restricted. So, he will lean forward with the upper body, by having tight hips, and strike the floor with the feet externally rotated, so all the body weight will be loaded in the middle of the foot. As a result, the Stability Joint that sits between the ankle and hip, so the knee, will compensate for the other two joint dysfunctions. In this case, the knees would take extra pressure medially and stretch out laterally. So, what should Mark do?! Well, initially, to stop the pain from happening, stopping running would be a good idea. Said so, that would not fix the problem. What Mark should do, is: Massage to boost the change within the tight joints and reduce the knee pain Start a mobility program to improve the Hip and Ankle functionality Exercises that aim to reduce tension in the external rotator reinforce the internal rotator (Gluteus Med and Min) Train on how to run These are the basic steps to implement a model of Mobility, Stability, and Strengthening. Does this model apply to other sports activities? Of course, it does. Visualise your body as a giant mechanical machine made of rope and hinges. The mechanical result will not be ideal if the hinges are stiff and the ropes are tight. To improve the result, each component needs to be looked after. So what message would be the most recommended? Along with Melbourne Massage and Treatment services, Thai Massage, Remedial Massage, and Myotherapy are soon the most recommended services Giovanni offers to improve the body’s mobility. Regarding mobility training, Thai Yoga is also an effective way to improve joint mobility, as these exercises focus primarily on improving joint mobility. What there is to consider is the patient’s presentation, medical history and pre-existent injuries. If there are no significant concerns, I suggest Thai Massage as the best approach. For people who have presentations such as Diabetes n1 or hypertension, Myotherapy treatment or Remedial Massage is mainly recommended.
A bunion is a bond malformation at the base of the big toes. The leading causes for bunion are: foot stress high foot arch wearing high heels narrow shoes A bunion is often correlated to Osteoarthritis. Osteoarthritis is due to the cartilage degeneration that separates 2 bonds. In this case, the 2 bonds are at the base of the big toes. This result in pain at big toe extension and during walking. Bunion’s Symptoms Visible malformation, like a bump, on the side of the big toes joint; Sharp pain in the thumb; Difficulties in walking; Stiffness; The big toes point laterally towards the other toes Intervention About what to do for a bunion presentation is to get in touch with a podiatrist as soon as possible. Massage therapy is recommended too, but it is a limited tool for helping in fixing the issue. Along with Remedial Massage, Thai Massage, Myotherapy and MLD treatment, what can be done to alleviate the pain is to treat the surrounding structures, such as the plantar of the foot and the metatarsal area. So, can it alleviate bunion pain and or invert the condition? Yes, it is. Today’s blog post is called “Happy Bunion Story”. So, back in Dec. ’21, Steph start having foot pain, due to osteoarthritis. The reasons behind her conditions are: High foot arch Long hour standing up for work (she is an amazing Wedding and Fashion photographer) Wearing high heels (she used to do modelling) The combination of those resulted in a degeneration of big toes cartilage and a bunion forming. As Steph complained about pain in the big toes, I told her what possibly was happening there. Soon after, she visited her GP and got some X-Ray done, and the result was not much of a surprise. After finding out about her new condition, Steph consulted a podiatrist, who suggested starting a daily routine of exercises for her big toes. Resisted big toes flexion (with a rubber band) Wearing spacer in between the toes Toes abduction from a seated position. But this is not all. The podiatrist even told her to wear an insole in her shoes. Furthermore, she was recommended to buy specific shoes that “protect her foot”. I saw the shoes myself, and I can tell you they didn’t look good. They were thick, big, and didn’t look comfortable to wear. Another podiatrist opinion A few months passed, and I went to see Andy, a podiatrist promoting barefoot wear for my own flat feet condition. As I was talking to Andy about my feet, I couldn’t resist getting an opinion in regard to what Steph was going through. Andy, without much hesitation, suggested that she wear barefoot shoes and continue the exercises. Next, we went down to Sole Mechanic, in Hampton, a shoe shop specialising in barefoot wear. Beforehand we researched different brands and decided to give a goal to the barefoot shoes, “Vivo Barefoot”. Sole Mechanic Experience The experience at Sole Mechanic was a positive one. We booked an appointment for 2 of us, 1 hour all up, so the staff has enough time to guide you through what barefoot is about and the best option. We went through the ankle and toes Range Of Motion and barometric platform test and tried a couple of shoes each. Vivobarefoot, given its ethical approach to shoe wear, was since the start our choice, and so far, the best option we could go for. At this stage, we have a couple of shoes each from Vivo barefoot, one for everyday wear and one for hiking. Back to the “Happy Bunion Story” So, after all this time, Steph now enjoys walking pain-free. The bunion, thanks to the exercises and to Steph’s determination in practising them daily and the new shoes that have a wider shoe box, is reduced, as the Big Toe is now diverging towards the medial side (away from the other toes). Osteoarthritis is a condition that can’t be fixed. Still, when Steph occasionally feels pain we do an MLD session which can help reduce the inflammation symptoms and help in pain management. Said so, the pain is a rare thing and not a daily issue. Furthermore, Steph is not wearing the insole anymore. As suggested by the Sole Mechanic staff, removing the insole is a process that can be done step by step. So, since Feb ’22 when we bought the first pair of Vivobearfoot shoes, took her approximately 2 to 3 months to abandon the insole, and now it is about three months that she is not using it anymore. Hopefully, this post gives you some hope and insights into what’s happening with bunions. If you are in pain and need to reduce the inflammation response to the bunion, MLD may be best for you as a short-term solution. Otherwise, book an appointment with Andy to find out the best way to adjust the shape of your foot as much as possible.
Myotherapy is a massage technique to treat or prevent soft tissue pain and restricted joint movement. “Myotherapy” stands for “Myo” Muscle “Therapy” therapy. In Australia, and specifically in Melbourne, it is a practice that took over the massage market in the last few decades and is not becoming more and more popular. There is Dry Needling and Joint Mobilization along the different techniques used in a Myotherapy treatment. Is Myotherapy Safe? Yes, Myotherapy is a safe treatment. Said so, you want to ensure that the therapist treating you has their qualification up to date. Here is a link to my qualification. What about Dry Needling in a Myotherapy Treatment? Dry needling is one of the many ways a Myotherapist can treat a client, but it is unnecessary. Before using needles, the therapist always has to double-check with the clients the following: No metal allergy No bleeding disorders No needle fear or phobia The client feels comfortable with such treatment The therapist does explain how dry needling works Is Myotherapy available at Melbourne Massage and Treatment? Yes, it is. I am a fully qualified Myotherapist who completed an Advance Diploma in Myotherapy at RMIT University. On top of all, I am now enrolled in the last year of my Bachelor’s Degree in the Myotherapy Clinic at Torrens University. What’s the difference between Myotherapy Treatment and Remedial Massage? Myotherapy is similar to a Remedial Massage session. The difference is that a Myotherapist has more knowledge about the human anatomy, joints, and functionality. So before the session, the therapist would guide the patient through a specific range of motion to evaluate the body’s presentation. Done so, the therapist has an idea of what can be done to improve the body’s presentation. Furthermore, a Myotherapist is trained to use mobilization, which is a repetitive joint movement to improve the joint’s range of motion. My favourite “mobs” are along the spine. They consist of a gentle push over the transverse process of the spine. Applying this constant firm push, the transverse process gain mobility, allowing all the muscle inserts originating from that joint to be more mobile. Is a mobilization the same as what a chiro does? No is not. The Chiro makes an adjustment, which is a fast joint pull or push, to adjust its position or functionality. Along with an adjustment, the patient has no control over the fast movement. Indeed, during mobilisation, the patient can take control of the push and stop the treatment if he/she does feel uncomfortable. Book Now your Myotherapy treatment with Giovanni. Giovanni is available in Fitzroy North at 175 Holden St Monday to Saturday 9 am to 7pm.
Muscle and Tendon are two types of fibres that connect bonds, allowing the joint to be moved by contracting or extending. Muscles and Tendons characteristics. A muscle consists of fibres of muscle cells covered by fascia, bundled with many more fibres, surrounded by thick protective tissue. So each muscle fibre is covered in the fascia, then wrapped as a whole muscle in more fascia. A tendon is a high-tensile-strength band of dense fibery connective tissue. Indeed tendons can transmit the mechanical forces of muscle to the skeletal system. Tendons, as per ligaments, are made of collagen fibres. Compared to a tendon, a muscle is elastic and sits in between 2 tendons parts which keep the muscle itself connected to bonds. So yes, muscles are not directly connected to bond themself. Luckily, there is to say, because if this was the case, it would be really easy to suffer from injuries like a muscle tear. Said so, it is now easy to understand that tendons are capable of holding more force. Injury type Due to the consistency of the tendon and its functionality, we can now understand why a tendon tear or rupture is a severe injury that requires surgical intervention and months of rehabilitation. On the other hand, often, after months of rehabilitation, still, the tendon would not go back to its original state. A common tendon rupture is Achille’s tendon. Achille’s tendon connects the lower part of the Gastrocnemius and Soleus to the foothill. Repetitive movement and repetitive partial load on this tendon are the leading cause of injury. Healthy muscle and tendon Simple and gentle exercises are a good way to keep your muscle and tendon out of trouble. The key points of these types of exercises are: Consistency Resisted load (by using rubber bands) Starting with light weight to then building up with time heavier load Good posture doing the exercises Have a day of rest from exercises once a week Avoid exercises that aggravate your pain. Said so, other critical points for muscle and tendons good health seating into: Having a good night’s rest Eating more fresh food than overprocessed food Regarding recovery from an injury, as previously mentioned in the ice pack and/or heat pack posts, the usage of temperature is recommended based on the stage of the injury and the pain experienced with it. Even though on an inflamed tendon, never apply a heat pack. Are you in need of treatment? Don’t look any further, and book your initial consultation by clicking here.
Lymph nodes (or lymph glands) are small lumps of tissue containing white blood cells that fight infection. They are part of the body’s immune system and filter lymph fluid, composed of water and waste products from body tissues. Introduction to Lymph Nodes Lymph nodes are located in different body areas. On average, we have approx 600 LN. In the neck area only, we find 160 LN itself. LN can vary in size and go from 2 to 30 mm. Lymph Nodes are connected by vessels, better known as afferent and efferent vessels. The afferent vessels carry the lymph to the lymph node, and the efferent vessels take the lymph away from the lymph nodes. So, the lymph nodes are also connected directly to the blood system, veins, and arteria. What is a lymph node made of? Despite the structures that enter and leave the lymph node, these cleaning stations are made of: Connective tissue capsule Supporting strands of connective tissue inside Below the marginal sinus, there are clusters of lymphocytes lymphoid follicles Artery, vein and nerve As for the filtering station, the lymph node is essential to ensure that no bacteria, viruses or dirt can access the blood system. Where we find no lymph nodes in the brain. Indeed, the lymph fluid around this area gets drained by the Optic and Olfactory nerve. Following then the position of the lymph nodes, we can define the watershed. MLD and Lymph Nodes. Lymph Nodes can occasionally be swollen, which happens when the body fights an infection. In my practitioner experience, I often have to refer to the lymph node concept to introduce the client to MLD treatment. Not many clients know about this technique; they are more familiar with Myotherapy or Thai Massage and Remedial Massage. Said so, the client who tried MLD are all well impressed with its benefit. During an MLD session, what happens is that with a gentle stretch and recoil of the skin, I help your lymphatic system to work faster. Consequently, that’s how swollen area gets reduced. In pushing your lymphatic system to work harder, the lymph node would receive more liquid to process. On the other hand, knowing where the lymph nodes are, is essential to ensure we push the lymph liquid in the right direction. If you haven’t booked your appointment yet and wish to set a goal for MLD, please follow this link.
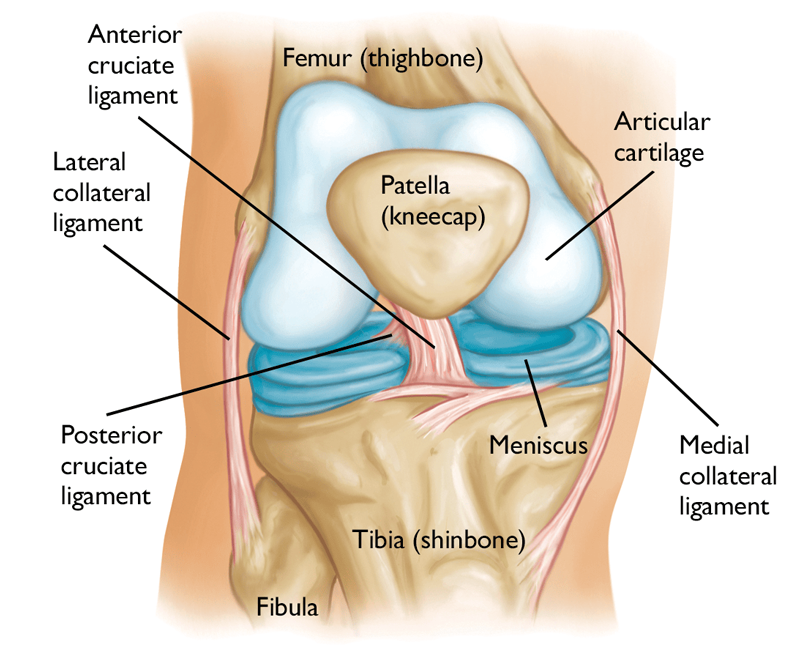
Knee pain is a common presentation for clients of any range of age and gender. Knee pain indeed is a vast topic. So in this post, we are going to go through how to identify the reason why we can experience knee pain. For doing so we are going to look at some special testing, that we use for the knee joints. Next, in a further post, we may analyse individual conditions. What about the Knee Joint? The knee is the strongest joint in the body. It takes a lot of pressure from the upper body and still has to handle the shock coming from the lower leg session, shock as walking, running and jumping. Indeed, whenever we do one of these actions, the knee plays a big role. Knee Anatomy Bond: Above: Femur Below: Medially the Tibia, laterally the Fibula. Patellar is the front “floating bond” Ligaments: Anterior Crucial Ligament Posterior Crucial Ligament Posterior Menisco-Femoral Ligament Fibular Collateral Ligament Tibial Collateral Ligament Transverse Ligament (this one is visible only from the front side of the knee, below the patella). In between the bonds we have: Medial Meniscus Lateral Meniscus If this post is talking to you, book your next massage session by clicking here. So, the knee joint can be divided into two parts: Tibiofemoral joint Connects through the collateral ligaments, cruciate ligaments and menisci; Patellofemoral joint Gives stability to the medial and lateral retinaculum and allows the extension mechanism through the tendons of the quadriceps f.. Now that we have a better idea of what the knee anatomy is, we can look into his functionality. Knee ROM are: Extension: 0° Flexion: 140° Internal Rotation: 30° External Rotation: 40° Abduction/Adduction: 15° Said so, we can see that the major movement that the knee can accomplish is, flexion. Even if the Internal and External rotation since to be a big move for the knee, in the reality, that’s not always the case. The older we get, easily this motion actively gets tighter. Indeed, one of the main reason for meniscus injury is the twisting of the knee, when the feet is holding the ground and the body rotates. But as previously mentioned in this post we would look into the knee special test. What knee functional test have to tell us? As we already mentioned in another post, a generic active, passive or resisted ROM tell us about muscle functionality. On the other hand, a special test for the knee can show us if a ligament or a meniscus is loose, in the case of ligament or injured. Furthermore, special tests, on the knee are essential to prevent further injury and reduce joint degeneration. To start with we have the drawer test: Anterior Draw test and Posterior Draw test. The Anterior one is to test the anterior crucial ligament, and the posterior, obviously, is for the crucial posterior ligament. Both these tests are done with the client lying supine on the table, with a hip and knee flexed, and foot on the table. The therapist will ensure that the foot doesn’t move and will place its hands around the knee, with the fingers (except the thumb) seating at the top of the calf and the thumbs seating on the patella. For the A.D. test, the therapist will lightly pull the knee joint away from the patient body. On the other hand, for the P.D. test, the therapist will push the knee towards the patient’s body. These tests are positive if there is a loose movement within the knee, in the direction of pull or push. If the client has a history of injuries, to the ACL or PCL the therapist wants to make sure not to push or pull with great effort, or injury could occur. Vagus and varus test. Those tests analyse the status of the medial and lateral ligaments. For the valgus test, the therapist places one hand above the knee laterally, and the other hand above the ankle on the medial side. By applying opposite pressure in the 2 directions we put the medial ligament under stress. If pain is reproduced, or there is a loose movement the test is positive. The same action is for the Varus test. In this case, the hands are placed still above the knee and ankle, but the bottom hand is placed laterally and the top one, is placed medially. Apleys Test This test is used to evaluate the state of the meniscus. The client, in this case, would be lying in a prone position, with the knee flexed. The therapist will be standing next to the client, on the side of the knee flexed and will apply pressure to the knee. If no pain is reproduced with pressure only, the therapist can gently apply a rotation movement to the flexed knee. The test is positive if the pain is reproduced. McMurray test. This is luckily the most efficient and most used knee test used by therapists in case of meniscus injury Here is how it works: The patient lies in the supine position with the knee completely flexed (heel to glute). Lateral Meniscus: the examiner then medially rotates the tibia and extends the knee. Medial Meniscus: the examiner then laterally rotates the tibia and extends the knee. McMurray is a positive test if the pain is reproduced. There are still a couple of tests that can be done for the knee, but so far we did cover the most important. About the therapy that I can offer for releasing knee pain, MLD is what I would suggest the most. Especially for acute pain and swelling or oedema reduction. Whereas, Myotherapy or Remedial Massage and Thai Massage can be used too but more to facilitate and or strengthen the muscle surrounding the area.
As already mentioned earlier MLD is a fantastic manual technique that can be used to improve the healing of many conditions. Along with the conditions that MLD is useful for there is bone fracture. Said so, in order to understand how MLD can help to speed up the recovery from a bone fracture we have to analyse what’s happening within the body when such trauma happens. A bone fracture is an injury that can happen at any age, due to an accident or trauma. The main type of bone fractures are: Displaced Angulated Shortened Rotate Symptoms of bone fracture Pain Swelling Bruising Deformity Inability to use the limb. The fracture so can be a crack side to side or in the middle of the bone. Eventually, the bone can crumble too, or break in multiple areas. At the worst, the bone can also cut the skin, and come out of the body. If this post is talking to you, book your next massage session by clicking here. Depending on where the fracture is, and what type of fracture it is, surgery could be required. Independently if surgery is required or not, still MLD can help to boost the recovery. Indeed, when a fracture happens the body recognises a trauma to its system. As long as the body won’t know exactly what the trauma is, and if the trauma does involve a skin crack or not, to prevent infections and external bacteria or pathogens to enter the body, the vein, capillaries and the lymphatic system around the trauma area get restricted. As per result, the body does swell. In fact, this explains why, when oedema happens the body does swell. It is an automatic body response to prevent further damage to happen. As the body then, realise what the issue is, slowly does reactivate the lymphatic system, and does fully reopen veins and capillaries, so that the blood can start circulating again freely. But the time that the body can reduce the swelling by itself, with a lymphatic system that works at regular speed (about 7 to 8 bits per minute) it would take a while to reduce the swelling. Furthermore, when I bone is broken that body part would have to stay still for a while, weeks or months. As per result, the blood and lymph flow would be slower than usual. And here is where MLD comes to be useful. If by reading this post, you feel like MLD is what you need now to recover from your injuries, click here to book now your next session. As MLD therapists indeed, we would check that there is no acute infection in the area where we want to apply MLD. If that’s the case, then, we can start our work. By boosting the lymphatic system, up to 3 to 4 times its normal ratio, we can quickly reduce the swelling. And what about if the area affected is covered with a plaster cast? Well, let’s not forget that the lymphatic system works as a vacuum and the area of loads is below the clavicle. So, stimulating the Lymphatic system at the top can actually already improve its suction ability till down the feet. For example, if the fracture is at the foot, initially MLD can be applied at the neck, to open the Lymphatic System duct that reverses in the veins, and secondly can be applied to the abdominal level and down the legs, just before the foot. Now, that swelling reduction, come’s with many benefits. For example, in the area treated, there is a transaction of extra oxygen, protein, vitamins, blood and other essential elements useful for the bone to heal. And occasionally, depending on the type of fracture is not only the bone the one that has to heal. In fact, along with a bone fracture, the body part fractured stays steel for weeks and months. That would create a weakness in the muscle that would then require rehabilitation. As a Remedial Massage therapist, I would have to refer the client to a Physiotherapist for rehabilitation. Even so, as a Remedial Massage therapist, I can still deliver massage services that can help in restoring muscle functionality. In conclusion, MLD can help with: reducing the swelling along a bone fracture; help in speeding up the recovery of the skin damaged by the fracture and or by the operation; Speeding up the healing of muscles and soft tissue around the fracture; Ultimately, by increasing relaxation, MLD is also useful to keep the humour of the person at ease, as often happens that after a trauma such as a bone fracture, the person can feel anxious and demoralised due to poor mobility and difficulties in moving.
- 1
- 2