“I was lifting the box from the floor, and then, ouch I did my back”! How often have you heard this? What’s going on here? Lower back pain is a common presentation that affects many people all around the world. But hurting your back when picking a box, or even a lightweight as the key, or tightening the shoes, is an injury that doesn’t affect only those with lower back pain. So to explain the mechanism behind these incidents, we have to look into what we call “proprioceptors”, specifically “muscle spindle”. Proprioceptors are body receptors within the skin, muscles and joints that reveal information about the body’s movement and send this information to the brain. How that information is transmitted to the brain is by different types of a pathway that we will see in a future post. In specific, today, we are going to look at the “muscle spindle”. So muscle spindles are proprioceptors that can tell the brain how the body is moving, specifically a muscle, and a proprioceptor that can tell a muscle to relax and change to stretch. Indeed, muscle spindles are different from other proprioceptors, as they can alter their sensitivity as needed. What did Muscle Spindles have to do with my back then? As mentioned above, a muscle spindle can alter muscle consistency. So, when banding forward to pick up the key or do the shoes lase, the back muscle must relax, as they have to stretch. But, if the muscle spindle doesn’t tell the back muscle to relax as you bend, those muscles will stay contracted, and guess what happens next? “Ouch, I did my back.” How to prevent the injury then? To prevent an injury as such, movement is the answer. Movement, as simple as a cat and cow exercise, would create that feedback response between your lower back area and the brain that, in the long term, would ensure your brain knows that when bending, the posterior portion of the body needs to be told to relax. Said so simple movement can prevent the injury, but further exercises, like a deadlift, can help your entire posterior chain to get stronger and get you to the next level of strengthening. But before lifting heavy weights, let’s not forget the importance of looking into mobility. In conclusion, to prevent this injury from happening, start moving. Incorporate regular breaks from your seating at the desk. Have a timer on your desk that, every 45 minutes, remind you to stand up, have a stretch and short walk, a water sip and get back to work. Book your next massage session at Melbourne Massage and Treatment if this post talks to you. How can Massage help? Massage therapy can help in different ways. First, it can help reduce the muscular tension within the lower back area. Second, the massage touch can help increase that body awareness, preventing further injury. The recovery process from an injury does depend from person to person. But within a few sessions within 1 to 2 months, using a mix of techniques, like MLD, Myotherapy and or Thai Massage, there is a good chance of good recovery and injury prevention. Exercises play an important role too in this recovery phase. How Many Sessions would I need? As already mentioned, everyone is different. Based on my experience, to help someone recover from an injury, initially, it can take up to 5 sessions spread over two months to achieve a good result. And again, this is not only about Massage but also about corrective exercises. Therefore, I offer a treatment plan allowing you to uptake five sessions of any treatment type at a discount rate of 10%. This offer is valid for returning clients who already had an initial consultation. This would allow me, as a therapist, to ensure I am the right therapist for you and that we can create a treatment plan that works for you and that you can use for your benefit.
Category Archives: Blog
I spent the last seven years achieving different massage qualifications to offer a service that is different from the standard massage. Why I started studying Massage therapy. My interest in the massage profession started as a curiosity and a desire for a career change. Indeed, before getting into the massage profession, I worked as Pizza Maker for a decade or so. That did allow me to get permanent residence in Australia. But I knew that hospitality life was not what I wanted to do for the rest of my life. So, in Jan 2016, I did enrol in a Certificate IV in Massage Therapy at the SSNT (Southern School of Natural Therapies) in Fitzroy. After that, as soon as I finished the course, I decided to go travelling and experience more of the outback life. It was not till February 2018 that I returned to studying massage practice. Thai Massage Qualification. That was in Chiang Mai, Thailand, with Pichest Boonthumme. I ended up in Chiang Mai, thanks to a friend who understood what I was looking for. And what was I looking for? Well, I was searching for someone to teach me more than a massage sequence or stroke. So I was not looking for just a random massage qualification. Someone that could show me how to improve myself as a massage therapist and person in the first place. Pichest is the right teacher. Anyway, I passed the first round of training in 2018 with Pichest, I then kept travelling, and before heading back to Australia, I did a second stopover in Chiang Mai, and that was in Jan 2019. But still, before starting the Diploma in Remedial Massage at the RMIT in July 2020, I did go to study with Pichest for another couple of weeks (November 2019). Do you feel like you need help with your neck pain? Book now your next appointment. Back to school. As already mentioned in 2020, in the full Covid-19 pandemic, I decided to completely abandon the hospitality industry and dive more into the massage practice. That’s why I did decide to go for a Remedial Massage course. Once the Remedial Massage course was over, in December 2021, I decided to step into the advance Diploma of Myotherapy, which would last one year more. Between those courses, I also found the time to take a class for MLD (Manual Lymphatic Drainage) with the Vodder Academy here in Australia. But, it was not till the latest training with Pichest Boonthumme (November 2022) that I understood how all those modalities are interconnected with the other one. Where am I now, along the massage qualifications journey? I just enrolled in the last year of my Bachelor of Health Science in Clinical Myotherapy at Torrens University. I did decide to enrol in this course for several reasons: Personal challenge. Learn more and more about body and massage practice. I am possibly going for a master’s after it (a master’s in acupuncture).
Here is a list of services available at Melbourne Massage and Treatment: Myotherapy Exercises Rehabilitation Remedial Massage Thai Massage MLD Thai Yoga What are these services about? First, any of those services are holistic services, so they can’t be official diagnoses for medical conditions, and Giovanni can’t prescribe any medications. What to expect is guidance on how muscularscaletol conditions, such as plantar fasciitis, tight muscle, muscle tear and more…can be looked after and overcome with manual therapy and exercises. As Myotherapist, Giovanni can guide you on how possibly the pain manifests and how with massage and specific exercises, the pain can be placed at ease. Part of the process of pain management is the change in habits. This can include posture at the workstation, but not only, but other changes can also include your training program, which maybe is too intense for your body and needs to be adjusted. How is the massage delivered? Any massage is delivered in total respect of the patient and the therapist. No nudity or sensual massage are available. Only the body area that needs attention would be exposed. The rest of the body is covered in a towel. Undress level is down to bra and underwear when need it. If we are working on your shoulder, there is no need to remove the pants. Regarding individual massage sessions, like myotherapy treatment, remedial massage, and/or Thai massage, an assessment of the muscular scale of the system would be delivered before the treatment. This assessment included a series of ROM. These assessments would help Giovanni understand what muscle or groups of muscles needs more attention during the treatment. What should I do before the massage session? Treatments such as myotherapy, remedial massage, and MLD include exposing the body parts that need to be worked on. Said so, having a shower before the treatment would be much appreciated. You don’t need to wear any perfume, a deodorant is enough. Should I shave? No, you don’t need to shave. If rock tape needs to be used, the rock tape can be placed over body hair. When you have to remove it, make sure to roll it downwards. Do not pull it off like it is a wax treatment. That could lead to ripping hair and skin off. Where does Giovanni work? Melbourne Massage and Treatment services are available at the Fitzroy North studio on Holden St. Book now your next appointment. If this post didn’t answer all your questions, don’t hesitate to message Giovanni through the Contact Page.
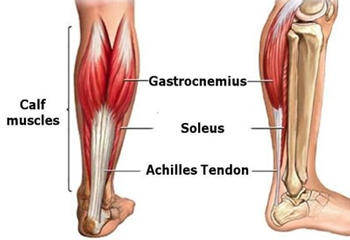
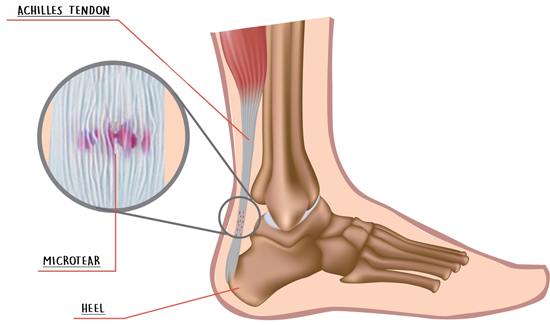
Achilles tendinopathy is a condition that manifests on the lower portion of the calf and is caused by overusing the muscle of this region, such as Gastrocnemius and or Soleus. Initially, you may not notice the issue, as it starts as a low-level inflammation and micro-tearing, but as the condition progresses, the damage and inflammation become more relevant. Achilles Tendinopathy can be easy to treat and manage when treatment is delivered in the early stages. If the injury is not looked after, the occurring damage could be much harder to resolve. Symptoms Most commonly, people experience pain in the morning or when the muscle is still cold. As the day progress and you start moving around, the pain may dissipate, and you start feeling better, ignoring the danger. Occasionally, the area would present swollen and or tender at the touch. Treatment options for Achilles Tendinopathy The management of this condition starts by improving the rest time and time off from sports activities, such as: Running Soccer Any sport which includes jumping or being on feet Other helpful approaches include: Heat pack Dry needling Improving Ankle and Big toes the mobility Massage Therapy Rock taping Achilles tendinopathies are not a condition that will heal on its own. As mentioned, it will feel better with rest, but as soon extra activities are played, the pain can back as strong as. Remedial Massage and or Myotherapy treatment can help target the painful area, stimulate an immune system response, and help with the recovery process. Also, along with the hands-on deep tissue work, mobilisation is a great way to reduce the tension in the ankle joint and improve the muscles’ functionality. After treatment, Giovanni will give you some exercises to take home. Those exercises would keep the area tension free, improve the joining mobility and strengthen the area.
As previously spoken in another blog post, sitting on the floor and working at the pc would be a better anatomical position than sitting on a chair. Why does sitting on the floor work better than sitting on a chair? Sitting on a chair is uncomfortable, especially in the long term. As a massage therapist, most of my clients are people who have cervical pain or suffer from headaches. Sitting at a desk for hours does more damage than you may realise. So, let’s start with the lower body portion. Staying seated on a chair does direct pressure on the thigh, and by doing so, muscles like the hamstring and gluteus muscles get compressed. By compressing this group of muscles, they get weak and stop functioning as they should. In addition, direct pressure is also applied to the sciatica nerve, the main nerve of the lower body portion. The piriformis often compresses the Sciatica nerve. This muscle runs beneath the Gluteus Max and connects the medial portion of the sacrum to the greater trochanter of the femur. So, the deactivation of those muscles would then manifest itself when we try to walk or, in any case, extend the leg. As the “firing pattern” blog post shows, the hamstring and gluteus max muscles are crucial in leg extension and help prevent lower back pain. This is what happens to the muscle part of the lower body portion. But this is not the only issue the body faces with so many hours sitting on a chair. There is more. So sitting on a chair does limit the body’s movement. The decline of the body’s movement creates a cascade of side effects, including mobility reduction in joints like the Hip, Ankle, Feet, and Thoracic. As all those joints don’t move, there is also a diminish in the proprioception body/brain. Another issue is the compensation of the stability joint over the mobility joint. Indeed, when a mobility joint gets stiff, the stability joint above and below would try to compensate. What’s a common finding pain-wise with sitting on a chair for long hours? The prevalent finding is a sore neck. The sore neck happens as the thoracic stuff up. Indeed the lower cervical portion of the vertebrae, which are stability joints, try to compensate for the thoracic stiffness and, in the long term, would cause neck pain, shoulder pain and headaches. Sitting on the floor can improve mobility. Sitting on the floor can help improve your mobility by allowing you to move your body in many different ways without the need to stand up. That movements are what your body needs as mobility exercises. That movement is your body’s way of improving its posture. Indeed, movement is a crucial component in pain prevention. And this doesn’t happen on a chair. How to switch habits? As for all the habit changes, this has to be gradual and not radical. So, start sitting on the floor for 1 hour a day. Give yourself the time to adapt to the change. Slowly you can incorporate more hours, but not in a row. Maybe one hour in the morning and one in the afternoon. Also, incorporate some standing time to sitting on the chair and floor. Implement change, too, within your training. You are doing something new, and your body needs to adapt. As shown in this clip, start, start implementing a habit of sitting on the floor by doing step-by-step movements: Step 1: Move one leg forward, and bend down the other knee. Step 2: Bring both knees down Step 3: Swing the lower leg to the side (either Lx or Rx) Step 4: Let your body weight go, and sit down Step 5: Now let your lower leg come forward and sit cross-leg. Step 6: Do from step 5 to step 1 in reverse By clicking here, and here you will find the links to a Thai Yoga exercise that can help a lot with improving hip mobility.
Fibromyalgia is a health condition that causes widespread pain and sensitivity to touch. This type of condition is more common in women than in men, and it is still unknown to science why some people may suffer from Fibromyalgia, even though it is known that stress can play a significant role. On the other hand, genetics can also be the reason why someone can suffer from Fibromyalgia. Fibromyalgia signs and symptoms Symptoms of fibromyalgia may include: headaches sleep disturbances numbness and tingling of the hands and feet muscle and joint stiffness after a period of rest (after sleeping) restlesconditionsndrome Diagnosis of fibromyalgia To be diagnosed with Fibromyalgia, you have to visit your GP first, who may refer you to a specialist. The most widely used clinical criteria for diagnosing fibromyalgia are sourced from the American College of Rheumatology: pain and symptoms over the past week, based on the total of: number of painful areas out of 18 parts of the body The severity of these symptoms: fatigue waking unrefreshed cognitive problems (that can be memory or thought) Plus other general physical symptoms Symptoms lasting at least 3 months, with unchanged Exclusion of other health problems that could reproduce the pain and other symptoms. Treatment and management So, currently, there is no direct cure for fibromyalgia, but there are many treatments that can help manage this condition, like: improving your sleep routine more of a balanced diet relaxation meditation exercise MLD You can also talk to your GP to see what medications can reduce or manage the pain. How MLD can help with Fibromyalgia? Manual Lymphatic Drainage (MLD) is a gentle, non-invasive manual therapy that aims at boosting the Lymphatic System. Along with the delivery of MLD, the therapist would gently stretch your skin and let the skin recoil, with a pain-free touch. This constant repetitive skin stimulation has a positive impact on the parasympathetic nervous system, which is the portion of the nervous system responsible for what we call “rest and digest” mode. Other benefits delivered from MLD are: Oedema reduction Deep relaxation Inflammation reduction Body’s fluid stimulation Skin health improvement Chronic pain management
Patellar tracking disorder is a condition that occurs when the patella, also known as the kneecap, moves out of its original place when the leg straightens or bends. What causes Patella Tracking Disorder? In most cases, the kneecap shifts towards the outside of your leg, called “Lateral Patella tracking”. Occasionally in some cases, it may shift toward the medial side too. Why this shift happens due to the force applied to the kneecap itself. It was said that the knee joint is a hinge joint, which connects the tibia and fibula of your leg with the femur. The kneecap is held in its natural position by ligaments on the medial and lateral sides and by tendons on the top side. Below the patella is a cartilage layer that helps the patella glide along the femur’s groove. When the cartilage below the patella does wear out, it can create pain and discomfort in the knee. The misalignment of the patella results from tendons, muscles or ligaments that are either too tight or too loose. Lateral patella tracking VS Medial patella Tracking In the case of Lateral Patella Tracking, the Vastus Lateralist is over-developed compared to the Vastus Medialis or the IT Band (Iliotibial Band) pulling too much. Vastus L. can overtake Vastus M’s strengthening due to the muscle size. Indeed the V.L. is visibly bigger than the V. M. On the other hand, tension along Gluteus Max and or tensions in the TFL can play a role in the pulling of the IT band. Are you in Pain, and you suspect to have a Patella Tracking disorder? Get in touch with Giovanni now. [contact-form][contact-field label=”Name” type=”name” required=”true” /][contact-field label=”Email” type=”email” required=”true” /][contact-field label=”Website” type=”url” /][contact-field label=”Message” type=”textarea” /][/contact-form] Risk factors for Patella Tracking Disorder Here is a list of reasons that can lead to Patella Tracking Disorder: Footwear Running Weakness in the quads muscle Unbalance of muscle between the inner and outer regions of your tight Sports that require excessive knee bending, jumping or squatting Improper form or techniques while working out or during sports activities Overweight Genetics (structural reasons) Incidents or trauma to the knees Malformation within the femur bond Damaged cartilage Symptoms Pain is the most symptom of Patella tracking disorder. The pain caused by this condition can occur during regular activity such as standing up, walking and or sitting down. Any knee movement can recreate the pain. In the case of arthritis, the pain can be more intense, and swelling is present at the knee joint. Treatment Options At Melbourne Massage and Treatment, the services available for Patella tracking are multiple. Depending on the severity of the condition, Myotherapy treatment and or MLD are the most recommended. Thanks to Dry Needling and/or Joint Mobilisation therapy, Myotherapy treatment can help rebalance the muscle forces surrounding the knee cap. On the other hand, MLD can help in reducing the inflammation and the swelling present eventually on the knee joint. What then Giovanni would look in, too, is also the mobility of ankles and hips. The correct mobility of these two joints would ensure that the knee is not compensating for the poor joint quality of movement, which can be part of why the patella tracking disorder is in the first place.
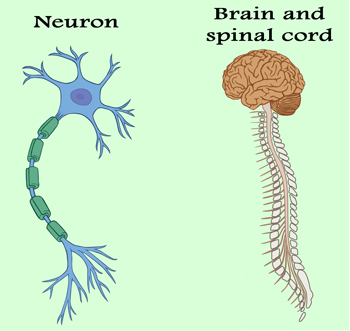
The Nervous System (NS) controls the voluntary and automatic functions of the body. It is made up of: brain spinal cord nerves Subdivision of the Nervous System The nervous system, initially, can be divided into the Central Nervous system (CNS), which is made of the Brain and Spinal Cord and the Perhiperic Nervous System (PNS), which consists of nerves that connect the CNS to the rest of the body. In more detail, the PNS can be divided into Sensory Neurons and Motor Neurons, the Motor Neurons can be divided into Somatic Neurons and Autonomic Neurons, and finally, this last is divided into the Sympathetic and Parasympathetic Nervous Systems. The function of the Nervous System The nervous system can also be defined by its functionality. For this subdivision, we have three categories: Sensory Affarent function Integrative function Motor Efferent Function The afferent function is characterised by a signal that travels to the brain from the PNS. The integrative part analyses the sensory information, stores some aspects, and makes decisions regarding appropriate behaviours. The Motor does respond to the stimulus by initiating an action. The Nervous System is made of Neurons. Neurons carry messages to and from different parts of the body. To be functional, neurons need three components: Oxygen Stimulation Food Neurons can start within the brain and travel down to the spine or can begin with the peripheric portion of the body and travel to the spine and brain next. Either way, the information can travel in one direction only. For afferent neurons, the direction is from the peripheric body portion to the brain, and the efferent is from the CNS or Brain to the peripheric part. Synapses connect neurons. The Synapse is the space where information is exchanged between two neurons. For a signal to be transmitted along a neuron, a chemical reaction has to happen within the neuron cell. This chemical reaction is better known as Action Potential. Once an Action Potential is started, an electric signal, within the order of mV would be transmitted from the Neuron cell to the opposite end, called Axon Terminal. At The Axon Terminal, the neurotransmitter would be passed and sent to the next neuron, receiving those substances through the receptors on its cell membrane. This is just a simplification of how communication between two neurons happens. In reality, there are variations to this communication methodology, and not always does the communication succeed. The NS is responsible for the following: memory, learning and intelligence movement controls the organs’ functions: – heart beating – breathing – digestion – sweating the senses: – sight – hear – taste – touch – smell The Sympathetic and Para-Sympathetic NS. The Autonomic NS controls the body parts we don’t have to think about it, like breathing, sweating or shivering, indeed the main organs. The SNS controls how we respond to emergencies. It makes our heart beat faster and causes the release of adrenaline. Where the parasympathetic nervous system prepares the body for rest (for example, when we go to sleep). The PSNS and the SNS work together to manage the body’s responses to our changing environment and needs. Massage and Nervous System As massage or manual therapy is a direct stimulus of the body, it plays a role in the response of the NS. What can happen is due to genetic factors, muscle tensions, and bulge disk nerves can get trapped along the way. Using the different testing approaches, such as Myotome and Dermatome, Giovanni can guide you through understanding where the nerve got entrapped or pinched. But this type of work is mainly for conditions where physically the nerve is involved in pour functionality. An example can be when someone has poor strength, on one hand, compared to the other, or when the sensitivity of a patch of skin is not so accurate. MLD and Nervous System Another technique, such as MLD (Manual Lymphatic Drainage), plays a role in the Parasympathetic Nervous System. An MLD treatment is profoundly relaxing, as it calms the nervous system, reduces pain and restores balance. This happens because of the mechanic repetitive movement used during the technique. There for, no pain has to be replicated during the treatment, or the SNS gets activated, as per pain response, and the body goes into “alarm” mode. Physical or mental pathologies can play a crucial role in the functionality of the nervous system, and techniques like MLD or Massage therapy generally can help in reducing symptoms and assisting in overcoming pain and body dysfunctions. Along the mental conditions, we find Anxiety or Depression too. In conclusion, any Massage Therapy or Manual Therapy, including Thai Massage, Remedial Massage, MLD and or Myotherapy, are great tools to release the tension in the body and improve the status of the nervous system. On the other hand, breathing, as per already disgust in the breathing wave blogs (Blog 1, Blog 2) plays a vital role in the well-being of the body, mind and nervous system. Feel stressed and need to release some tension? Book now your next massage at Melbourne Massage and Treatment.
On the occasion of my 4th time in Chiang Mai, since 2018, I am dedicating this post to Thai Massage in Pichest Boonthumme Style. When and where did it all start? In March 2018, I started studying and practising Thai Massage. I came here to Chiang Mai, to see Pichest Boonthumme, after a friend’s recommendation. I was looking into finding someone, that could teach and share a massage technique, not only based on sequence and repetitive movement. As often happens, as long as you ask, what you are looking for will show up. And now, after 3 long years of the Covid pandemic and limitations on travelling, I am back in Chiang Mai. This is my first trip out of Australia since 2019, so it was an excellent way to celebrate the freedom of travelling, once again. Being back at Pichest Thai Massage School is always challenging. Even though I spent the last three years training for Remedial Massage, Myotherapy and MLD, when I came here, there was always something new to learn. Along with that new practice, there is always the Thai/Buddhist philosophy aspect of how to see things. I did really like the way Pichest, with his limited English, can explain the complex way life can present and shape, and how simple it is to learn how to deal with it. Just observe the breath. Well, no surprise, as this is the principle of Vipassana Meditation itself. That said, what most often happens is that people who come here to study with Pichest ask to learn how to breathe, even before they can receive a massage. Many people come here because they heard of how good Pichest is at giving massages. And they all come with the expectation to get fixed. And it is just hilarious to see how Pichest, every time, turn these people away from treatment and asks them to learn how to breathe. We are used to thinking of Thai Massage as a painful approach, a strong technique, and it is. But not because we are physically suffering means we are getting better. If we can’t deal with the pain if we stop breathing as we perceive that pain, we keep creating tension in the body and will not let the healing process happen. Breathing during a massage comes with a series of benefits: helps the blood to be pushed around Oxygenation of the muscle tissues Improve relaxation It helps in dealing with the pain reproduced by the touch of a tense area Stimulates the Vagus Nerve, which controls the parasympathetic nervous system On the other hand, before we start doing deep work on the body, the patient does better take 5 minutes to practice breathing, and the first area to work would be around the posterior portion of the shoulder and the hip or Tibia area, to stimulates the blood flow within the body. In conclusion, Thai Massage as we know it in the West is a bit of a distortion of the real thing. Thai Massage, as with any deep tissue massage, can replicate pain, but the pain must be good, not sharp. The pain must help to release tensions and not increase them. And to be a Thai Massage therapist, you better know your anatomy well. Are you curious to find out what a traditional Thai Massage is like? Bookings are open for Traditional Thai Massage at Melbourne Massage and Treatment Fitzroy North studio.
Frozen shoulder is also known as per the name “adhesive capsulitis”. A frozen shoulder as per the name is a shoulder that would barely move. Both signs and symptoms typically begin slowly and then get worse. Recovery time is subjective. Causes and Symptoms of frozen shoulder. Causes A common cause of a Frozen Shoulder is having to keep a shoulder still for an extended period, like after an accident. Even if it is not clear yet why there are also psychosomatic reasons why a shoulder can get frozen. Another reason why a shoulder could get to freeze is traumatic events, such as a high level of stress or a physical accident. On the physical level, what happen is that connective tissues that surround the shoulder joint, like a capsule, thickens and tightens around the shoulder joint, and by doing so, it does restrict the joint’s movement. Symptoms Frozen Shoulder symptoms developed in 3 different stages. The stage’s timing is subjective. Freezing stage Shoulder range of motion starts decreasing, and pain shows up/increases. Frozen stage The Shoulder would freeze up. The movement is minimal, even though it is less painful. Thawing stage In this stage, the range of motions are slowly coming back Pain can be worst at night. This may happen because of the sleeping position or because the sensory feeling is more acute at night than in the daytime when the body perceives more sensations. Suffering from Frozen Shoulder and need some help. Book now an MLD treatment at Melbourne Massage and Treatment. Risk factors for Frozen Shoulder Age and gender Women are more luckily to suffer from this condition. Also, age plays a crucial role in this type of pathology. People 40 and over are luckier indeed to develop F.S. Systemic diseases Here is a list of specific conditions that can increase the possibility of suffering from F.S.: Diabetes Overactive thyroid (hyperthyroidism) Underactive thyroid (hypothyroidism) Cardiovascular disease Parkinson’s disease Prevention There are not many preventive factors when it gets to F.S. This is because the main cause of F.S. is holding the shoulder back from doing movements, due to a previous injury, most of the time. What can help, and this is how Melbourne Massage and Treatment services come in handy is to do MLD sessions on the area surrounding the injury. How MLD can help by stimulating the lymphatic system work and boosting the recovery process. Also, MLD would help in reducing inflammation. Other massage technique such as Myotherapy or Remedial Massage and or Thai Massage, is not as effective for this type of condition. Another successful method that can help once Frozen Shoulder is already developed is by using Hydrodilatation. This methodology consists in injecting sterile water into the joint capsule to stretch the open space and bring the shoulder back to its ROM.